Benefits of an Electronic Medical Record System
An electronic medical record system (EMR) offers numerous benefits to healthcare providers, patients, and the overall healthcare system. By transitioning from paper-based records to an electronic system, healthcare organizations can streamline their operations, enhance patient care, and improve efficiency. Here are some key benefits of implementing an electronic medical record system:
1. Improved Accessibility: With an EMR system, healthcare providers can access patient records anytime and anywhere, eliminating the need to search through stacks of paper files. This allows for quick access to critical patient information, resulting in more efficient and informed decision-making.
2. Enhanced Patient Care: EMR systems facilitate better coordination and communication among healthcare professionals, leading to improved patient care. Healthcare providers can easily share patient information, test results, and treatment plans, ensuring continuity of care across different healthcare settings.
3. Reduced Errors: Electronic medical record systems minimize the risk of errors commonly associated with manual record-keeping. Illegible handwriting, missing data, and misplaced files are eliminated, reducing the chances of medication errors, misdiagnoses, and treatment delays.
4. Increased Efficiency: EMRs automate various administrative tasks, freeing up healthcare providers’ time to focus on patient care. Functions like appointment scheduling, billing, and prescription management can be streamlined, reducing paperwork and enhancing overall efficiency.
5. Cost Savings: While the initial implementation costs may be significant, EMR systems can lead to long-term cost savings. With streamlined processes, reduced paperwork, and improved accuracy, healthcare organizations can save on storage space, supplies, and operational expenses.
6. Data Analytics: EMR systems can generate valuable data for analysis purposes. Healthcare organizations can use this data to identify trends, monitor health outcomes, and improve population health management. It also enables better decision-making regarding resource allocation and quality improvement initiatives.
7. Improved Patient Engagement: EMRs offer patient portals that allow individuals to access their own health records, including lab results, appointment schedules, and medication information. This empowers patients to take an active role in their healthcare, leading to better engagement and improved outcomes.
8. Enhanced Communication: Electronic medical record systems facilitate secure and efficient communication among healthcare providers. It allows for quick sharing of information, collaboration on treatment plans, and timely updates, leading to improved patient safety and care coordination.
9. Regulatory Compliance: EMR systems help healthcare organizations adhere to regulatory requirements and standards. They provide features like automatic coding and documentation templates, ensuring compliance with billing and reporting regulations.
10. Continuity of Care: EMR systems enable the seamless transfer of patient information between healthcare providers, ensuring continuity of care. This is especially crucial when patients are referred to specialists or transferred between different healthcare facilities.
In summary, implementing an electronic medical record system offers numerous benefits, including improved accessibility, enhanced patient care, reduced errors, increased efficiency, cost savings, data analysis capabilities, improved patient engagement, better communication, regulatory compliance, and continuity of care. It is clear that transitioning to an EMR system is a worthwhile investment that can significantly transform and improve healthcare delivery.
Components of an Electronic Medical Record System
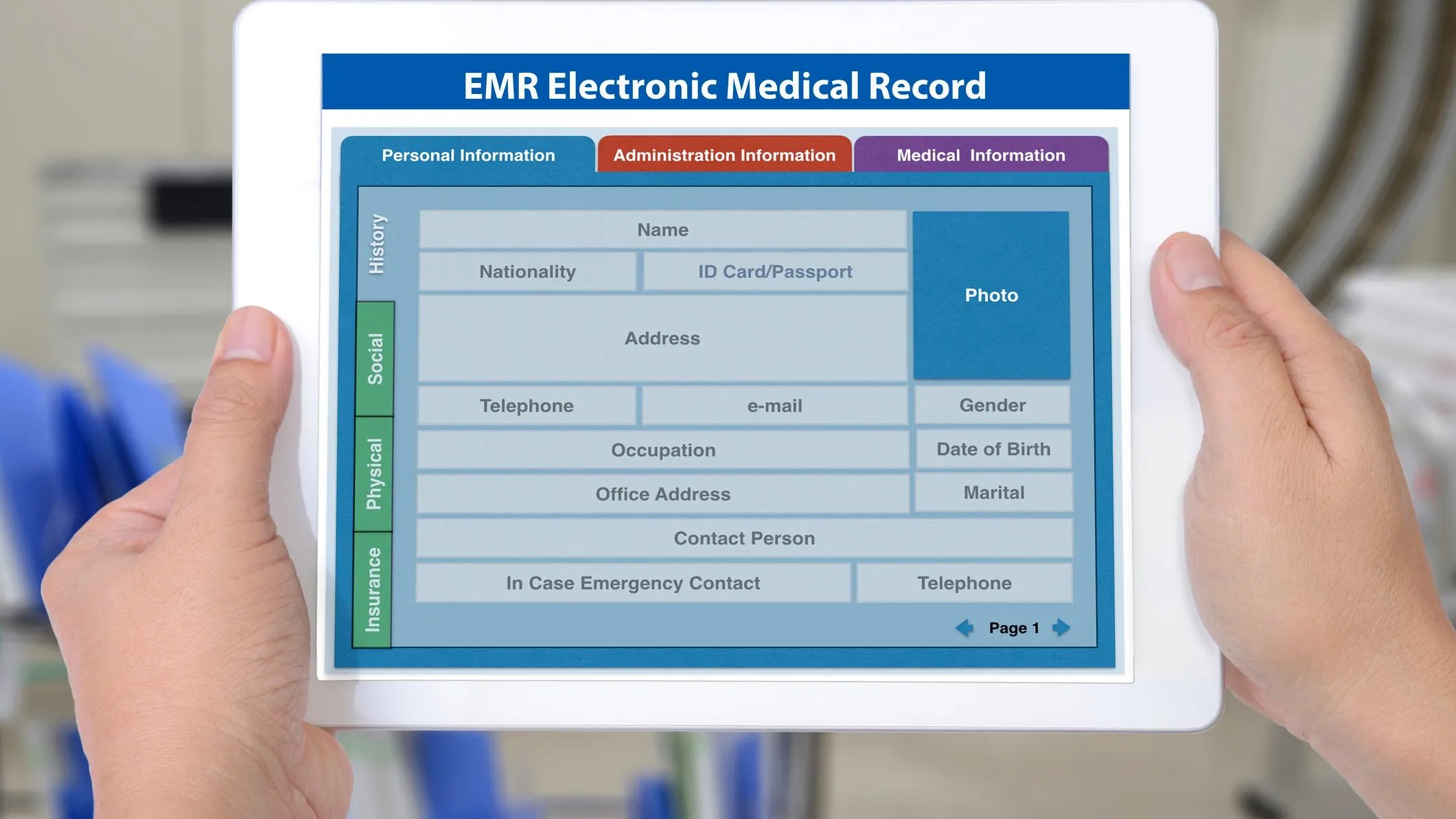
An electronic medical record system (EMR) consists of several key components that work together to store, manage, and retrieve patient information efficiently. These components ensure the smooth functioning of the EMR system and play a vital role in improving workflow and patient care. Here are the primary components of an electronic medical record system:
1. Electronic Health Records: The core component of an EMR system is the electronic health record (EHR). This is a digital version of a patient’s medical records, including demographic data, medical history, allergies, lab results, medications, and treatment plans. The EHR serves as a comprehensive record of a patient’s health information and is easily accessible by authorized healthcare providers.
2. Computerized Provider Order Entry (CPOE): CPOE enables healthcare providers to enter medical orders electronically, including prescriptions, tests, and procedures. This component eliminates the need for handwritten orders, reducing errors and facilitating accurate and timely communication between healthcare providers and other departments.
3. Laboratory Information System (LIS): The laboratory information system is responsible for managing laboratory test orders, results, and data. It ensures seamless integration and communication between the EMR system and the laboratory, allowing for quick and accurate access to lab results by healthcare providers.
4. Patient Portal: The patient portal component allows patients to access their own health information securely. Patients can view lab results, request prescription refills, schedule appointments, and communicate with healthcare providers. The patient portal enhances patient engagement and promotes active involvement in their healthcare.
5. Practice Management System (PMS): The PMS component is responsible for managing administrative tasks, such as appointment scheduling, billing, and claims processing. It integrates with the EMR system to ensure smooth coordination between clinical and administrative processes, improving operational efficiency.
6. Decision Support System: The decision support system provides healthcare providers with clinical decision support tools, such as drug-drug interaction checks, dosage calculators, and clinical guidelines. This component enhances patient safety, improves treatment outcomes, and ensures adherence to evidence-based practices.
7. Interoperability: Interoperability is a critical component of an EMR system, enabling seamless data exchange between different healthcare systems and providers. It allows for the integration of data from external sources, such as laboratories, pharmacies, and imaging centers, ensuring a complete and accurate patient record.
8. Security and Privacy Measures: The security and privacy component includes measures to protect patient information from unauthorized access, breaches, and data loss. This includes robust authentication protocols, encryption methods, data backup systems, and adherence to regulatory guidelines, such as HIPAA.
9. Mobile Access: Many EMR systems now offer mobile access, allowing healthcare providers to access patient information on smartphones and tablets. This component enables remote access to patient records, enhances care coordination, and improves flexibility in delivering patient care.
In summary, the components of an electronic medical record system include the electronic health record, computerized provider order entry, laboratory information system, patient portal, practice management system, decision support system, interoperability, security and privacy measures, and mobile access. These components work together to create a comprehensive and efficient EMR system that enhances workflow, patient care, and overall healthcare delivery.
Key Features of an Electronic Medical Record System
An electronic medical record system (EMR) is equipped with various features that enable healthcare providers to efficiently manage patient records, enhance clinical workflow, and improve the overall quality of patient care. These key features provide the foundation for an effective EMR system. Here are some essential features of an electronic medical record system:
1. Document Management: EMR systems allow healthcare providers to store, manage, and access patient records electronically. This feature eliminates the need for paper-based charts and ensures that medical records are organized, easily searchable, and readily available.
2. Electronic Prescribing: Electronic prescribing is a feature that enables healthcare providers to electronically generate and send prescriptions to pharmacies. This feature improves medication safety by reducing errors, ensuring accurate dosing, and providing real-time access to allergy and drug interaction information.
3. Order Entry and Results Management: EMR systems include functionality for healthcare providers to enter medical orders electronically and manage the processing of those orders. This feature facilitates quick and accurate order entry and streamlines the management of test results, ensuring timely access to crucial diagnostic information.
4. Clinical Decision Support: EMR systems incorporate clinical decision support tools that offer real-time, evidence-based guidance to healthcare providers. These tools provide alerts, reminders, and suggestions to help clinicians make informed decisions about diagnoses, treatments, and preventive care.
5. Interoperability: Interoperability is a critical feature that allows EMR systems to exchange data with other healthcare systems and providers. This feature enables seamless sharing of patient information, promotes care coordination, and facilitates the integration of external data sources, such as laboratory results and imaging studies.
6. Health Information Exchange: EMR systems support health information exchange, allowing healthcare providers to securely share patient data with other authorized entities. This feature is beneficial for referrals, consultations, and transitions of care, ensuring that all relevant healthcare providers have access to comprehensive and up-to-date patient information.
7. Workflow Management: EMR systems offer features to optimize clinical workflow and streamline administrative processes. This includes appointment scheduling, task management, and automated workflows, minimizing manual tasks and improving efficiency in healthcare delivery.
8. Reporting and Analytics: EMR systems provide reporting and analytics capabilities that allow healthcare organizations to track and analyze clinical, operational, and financial data. This feature enables data-driven decision-making, facilitates quality improvement initiatives, and supports population health management.
9. Patient Engagement: EMR systems incorporate tools for patient engagement, such as patient portals and secure messaging. These features enable patients to access their own health information, communicate with healthcare providers, and actively participate in their care.
10. Security and Privacy: EMR systems include robust security features to ensure the confidentiality, integrity, and availability of patient information. This includes authentication mechanisms, data encryption, audit trails, and compliance with privacy regulations.
In summary, the key features of an electronic medical record system include document management, electronic prescribing, order entry, clinical decision support, interoperability, health information exchange, workflow management, reporting and analytics, patient engagement, and security and privacy measures. These features collectively enhance the efficiency, safety, and quality of patient care, enabling healthcare providers to deliver optimal healthcare services.
Types of Electronic Medical Record Systems
There are different types of electronic medical record (EMR) systems available, each with its own unique features, functionality, and deployment models. Healthcare organizations can choose the type of EMR system that best suits their specific needs and requirements. Here are some common types of electronic medical record systems:
1. Web-based EMR: Web-based EMR systems, also known as cloud-based EMRs, are hosted on remote servers and accessed through a web browser. These systems offer flexibility and accessibility as they can be accessed from any device with an internet connection. Web-based EMRs are typically managed by third-party vendors, who handle system maintenance, data backups, and security.
2. Client-Server EMR: Client-server EMR systems are installed on a local server within the healthcare organization’s premises. These systems require dedicated hardware and IT infrastructure to store and manage patient data. Client-server EMRs provide greater control and customizability but require ongoing maintenance and IT support.
3. Mobile EMR: Mobile EMR systems are designed to be accessed on smartphones and tablets, providing healthcare providers with mobility and flexibility. These systems offer features such as mobile documentation, e-prescribing, and secure messaging. Mobile EMRs can be web-based or require the installation of a mobile app.
4. Specialty-specific EMR: Specialty-specific EMR systems are tailored to meet the specific needs of a particular medical specialty or practice. These systems offer specialized templates, workflows, and clinical decision support tools designed for specific areas of healthcare, such as cardiology, pediatrics, or dermatology.
5. Enterprise EMR: Enterprise EMR systems are designed for large healthcare organizations that have multiple facilities and departments. These systems provide a centralized platform for sharing and managing patient information across different locations. Enterprise EMRs enable seamless data exchange and care coordination among various healthcare providers within the organization.
6. Integrated EMR: Integrated EMR systems are designed to integrate with other health information technology (HIT) systems, such as a laboratory information system (LIS), picture archiving and communication system (PACS), and pharmacy management system (PMS). These systems facilitate the exchange of data between different systems, ensuring a comprehensive view of patient information.
7. Open-source EMR: Open-source EMR systems are built on publicly available source code, allowing users to modify, customize, and enhance the system according to their specific needs. Open-source EMRs provide flexibility, cost-effectiveness, and a collaborative community for ongoing development and support.
8. Small Practice EMR: Small practice EMR systems are designed specifically for small medical practices with limited resources and staff. These systems typically offer basic functionalities, such as patient demographics, appointment scheduling, and billing, while being user-friendly and cost-effective.
It’s important for healthcare organizations to carefully evaluate their requirements and consider factors such as scalability, customization options, integration capabilities, security, and support when choosing the type of EMR system.
In summary, the types of electronic medical record systems include web-based EMRs, client-server EMRs, mobile EMRs, specialty-specific EMRs, enterprise EMRs, integrated EMRs, open-source EMRs, and small practice EMRs. Each type offers unique features and deployment models to meet the diverse needs of healthcare organizations.
Common Challenges in Implementing Electronic Medical Record Systems
Implementing an electronic medical record (EMR) system in a healthcare organization is a complex process that comes with its own set of challenges. While the benefits of EMR systems are undeniable, it’s crucial to be aware of and address these challenges to ensure a successful implementation. Here are some common challenges in implementing electronic medical record systems:
1. Resistance to Change: Resistance to change is a significant challenge when transitioning from paper-based records to an EMR system. Healthcare professionals, especially those who are accustomed to traditional methods, may resist adopting new technologies and workflows. Overcoming this resistance requires effective communication, training, and ongoing support to help users understand the benefits of the EMR system.
2. Limited User Training: Insufficient or inadequate user training can hinder the successful implementation of an EMR system. Users need comprehensive training on the features, functionalities, and workflows of the EMR to ensure proper utilization and maximize the system’s benefits. Investing in comprehensive training programs and providing ongoing support is essential for user adoption.
3. Data Migration and Integration: Transitioning from paper records to an electronic system involves the conversion and migration of existing data. This process can be challenging, especially when dealing with large volumes of data and ensuring the accuracy and integrity of the migrated information. Integrating the EMR system with other health information technology systems, such as labs and pharmacies, also requires careful planning and coordination.
4. Workflow Disruptions: Implementing an EMR system can disrupt existing workflows, causing temporary productivity decreases and potential confusion among healthcare staff. It’s essential to carefully analyze and redesign workflows to align with the capabilities of the EMR system, minimizing disruptions and ensuring smooth transitions.
5. Cost and Financial Considerations: Implementing and maintaining an EMR system can be costly, especially for smaller healthcare organizations. There are upfront costs associated with software licensing, hardware infrastructure, training, and ongoing maintenance expenses. Evaluating the financial impact and developing a realistic budget is crucial for successful implementation and long-term sustainability.
6. Technical Challenges: EMR implementation can pose technical challenges, including hardware and software compatibility issues, system downtime, and data security concerns. It’s important to work with experienced IT professionals and vendors who can address these challenges and provide necessary technical support.
7. Change Management: Change management is crucial for successful EMR implementation. It involves effectively communicating the benefits of the EMR system, addressing concerns, and engaging stakeholders at all levels. Developing a change management plan that includes clear goals, timelines, and strategies for stakeholder involvement is essential for a smooth transition.
8. Interoperability and Data Standardization: Achieving interoperability among different healthcare systems and ensuring standardized data formats can be challenging. Data exchange protocols, such as Health Level Seven International (HL7) standards, need to be implemented and coordinated with external entities to ensure seamless data sharing and continuity of care.
9. Workflow Customization: Balancing the need for standardized workflows with the need for customization to meet specific organizational requirements can be a challenge. An EMR system should be flexible enough to accommodate different clinical practices and specialties while maintaining standardized processes for data capture and reporting.
10. Long-Term System Optimization: EMR systems require ongoing maintenance, updates, and optimization to ensure their continued effectiveness. It’s important to establish a governance structure and allocate resources for continuous system improvements, user feedback, and addressing system limitations.
In summary, implementing an electronic medical record system comes with common challenges such as resistance to change, limited user training, data migration and integration, workflow disruptions, cost considerations, technical challenges, change management, interoperability and data standardization, workflow customization, and long-term system optimization. Understanding and addressing these challenges proactively are crucial for a successful EMR implementation and the realization of the system’s benefits.
Considerations for Choosing an Electronic Medical Record System
Choosing the right electronic medical record (EMR) system is a critical decision for healthcare organizations. With numerous options available in the market, it’s important to consider several factors to ensure that the chosen EMR system meets the specific needs and requirements of the organization. Here are some key considerations to keep in mind when choosing an electronic medical record system:
1. Functionality: Assess the functionality and features of the EMR system to ensure it meets the specific needs of your organization. Consider features such as electronic prescribing, clinical decision support, order entry, documentation templates, reporting and analytics, and patient engagement tools. The system should support the workflow and processes of your healthcare organization.
2. Integration and Interoperability: Evaluate the system’s ability to integrate with other health information technology systems, such as laboratory information systems, pharmacy management systems, and picture archiving and communication systems. Seamless interoperability ensures the exchange of information and promotes care coordination across different healthcare providers and organizations.
3. Scalability: Consider the scalability of the EMR system to accommodate the organization’s future growth and expansion. The system should be able to handle increasing volumes of data, support additional functionalities, and seamlessly integrate with new technologies.
4. Usability and User Experience: Assess the user-friendliness and intuitiveness of the EMR system. The system should have a user-friendly interface, easy navigation, and logical workflows. User feedback and input from healthcare professionals during the evaluation process can help determine the system’s usability.
5. Vendor Support and Training: Research the vendor’s reputation and their commitment to customer support and training. Ensure that the vendor provides comprehensive training and ongoing support to healthcare staff during implementation and beyond. Prompt and effective technical support is crucial for the smooth functioning of the EMR system.
6. Security and Privacy: Evaluate the system’s security measures and adherence to privacy regulations, such as HIPAA. Consider features such as role-based access control, data encryption, audit trails, and disaster recovery capabilities to ensure the confidentiality and integrity of patient information.
7. Cost and Return on Investment: Consider the total cost of ownership, including upfront costs, ongoing maintenance expenses, and potential savings or revenue generated by the system. Assess the potential return on investment, such as increased efficiency, reduced errors, improved patient outcomes, and better revenue management.
8. Vendor Stability and Longevity: Evaluate the vendor’s financial stability, reputation in the industry, and the longevity of their product and support services. This ensures that the vendor will continue to enhance and support the EMR system over the long term.
9. Regulatory Compliance: Ensure that the EMR system complies with relevant regulatory requirements, such as meaningful use criteria, certification standards, and industry guidelines. It should support necessary reporting and documentation to meet regulatory obligations.
10. User Feedback and References: Seek user feedback and references from other healthcare organizations that have implemented the EMR system. Learn about their experiences, challenges, and the system’s effectiveness in meeting their needs. This firsthand information can provide valuable insights during the evaluation process.
In summary, choosing an electronic medical record system requires careful consideration of functionality, integration and interoperability, scalability, usability, vendor support and training, security and privacy, cost and return on investment, vendor stability and longevity, regulatory compliance, and user feedback. A thorough evaluation process based on these considerations will help healthcare organizations select an EMR system that aligns with their goals and facilitates optimal healthcare delivery.
Security and Privacy of Electronic Medical Record Systems
Ensuring the security and privacy of patient information is of utmost importance when it comes to electronic medical record (EMR) systems. Healthcare organizations must prioritize robust security measures to protect sensitive health data from unauthorized access, breaches, and information leaks. Here are some key considerations for the security and privacy of electronic medical record systems:
1. Data Encryption: EMR systems should utilize strong encryption methods to protect sensitive data both in transit and at rest. Encryption scrambles the data, making it unreadable to unauthorized individuals and ensuring that even if data is intercepted, it remains secure.
2. Role-Based Access Control: Implementing role-based access control ensures that only authorized individuals have access to patient records. This feature restricts access to sensitive information based on the user’s role, responsibilities, and the “need-to-know” principle.
3. Audit Trails and Logging: EMR systems should maintain detailed audit trails and logs that record all system activities and user actions. This enables healthcare organizations to track and monitor access to patient records, detect unauthorized access attempts, and investigate any suspicious activities.
4. Physical Security Measures: Protecting the physical infrastructure where the EMR system is housed is essential. Measures such as restricted access to server rooms, video surveillance, and environmental controls (e.g., fire suppression systems) should be in place to prevent unauthorized physical access and safeguard against physical threats.
5. Authentication and Password Policies: Strong authentication measures, such as two-factor authentication or biometric authentication, should be implemented to verify the identity of users accessing the EMR system. Additionally, enforcing strong password policies, including regular password changes and complexity requirements, helps safeguard against unauthorized access.
6. Disaster Recovery and Data Backup: EMR systems should have robust disaster recovery plans in place to ensure data availability and minimize system downtime in the event of a disaster. Regular data backups should be performed to prevent data loss and facilitate quick recovery in case of any system failures or incidents.
7. Staff Training and Awareness: Healthcare organizations should prioritize staff training and awareness programs to educate employees about the security and privacy policies, best practices, and potential risks associated with EMR systems. Training should cover topics such as phishing attacks, handling of sensitive information, and proper use of the EMR system.
8. Compliance with Privacy Regulations: EMR systems should comply with relevant privacy regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States. Compliance includes safeguarding protected health information (PHI), notifying patients of privacy practices, and providing individuals with the right to access and amend their health information.
9. Vendor Security Measures: Evaluate the security practices and measures implemented by the EMR system vendor. This includes assessing their data protection policies, security audits, employee background checks, and adherence to industry best practices and standards.
10. Regular Security Assessments: Perform regular security assessments, such as vulnerability scans and penetration testing, to identify any potential weaknesses or vulnerabilities in the EMR system. Addressing these vulnerabilities promptly helps prevent security breaches and ensures the ongoing security of patient information.
In summary, ensuring the security and privacy of electronic medical record systems requires robust measures such as data encryption, role-based access control, audit trails and logging, physical security measures, authentication and password policies, disaster recovery and data backup, staff training and awareness, compliance with privacy regulations, vendor security measures, and regular security assessments. Implementing these measures helps safeguard patient information and instills trust in the healthcare organization’s commitment to maintaining the confidentiality and privacy of sensitive health data.
Integration of Electronic Medical Record Systems with other Health IT Systems
Integration of electronic medical record (EMR) systems with other health information technology (IT) systems is crucial to ensure seamless communication and data exchange among various healthcare stakeholders. Integration enhances care coordination, improves workflow efficiency, and enables healthcare organizations to deliver optimal patient care. Here are some key considerations for integrating EMR systems with other health IT systems:
1. Laboratory Information Systems (LIS): Integration with LIS enables the electronic transmission of lab orders and results between the EMR system and the laboratory. This integration streamlines the lab testing process, ensures accurate and timely access to lab results, and facilitates clinical decision-making.
2. Pharmacy Management Systems (PMS): Integrating EMR systems with PMS allows for electronic prescribing, medication management, and real-time access to medication history. This integration reduces medication errors, improves medication reconciliation, and enhances medication safety.
3. Picture Archiving and Communication Systems (PACS): Integration with PACS allows healthcare providers to access and view radiology images and reports directly from the EMR system. This integration improves diagnostic accuracy, eliminates the need for manual image retrieval, and enhances collaboration among radiologists and referring physicians.
4. Health Information Exchanges (HIE): Integration with HIEs enables the secure exchange of patient health information between different healthcare organizations. This integration promotes care continuity during transitions of care, facilitates access to comprehensive patient information, and enhances care coordination across different healthcare settings.
5. Electronic Prescribing of Controlled Substances (EPCS): Integration with EPCS systems allows for the electronic prescribing of controlled substances, following strict regulatory requirements and security measures. This integration reduces paper-based prescriptions, improves prescription accuracy, and enhances monitoring of controlled substance prescriptions.
6. Telehealth Systems: Integrating EMR systems with telehealth platforms enables seamless documentation, billing, and access to telehealth visit information. This integration supports remote patient monitoring, virtual consultations, and telehealth-based care delivery.
7. Patient Portals and Personal Health Records (PHR): Integration with patient portals and PHRs empowers patients to access and manage their health information. This integration allows patients to view lab results, schedule appointments, communicate with healthcare providers, and actively participate in their care.
8. Revenue Cycle Management (RCM) Systems: Integration with RCM systems facilitates accurate and streamlined billing processes, coding automation, and claims management. This integration improves financial performance, reduces billing errors, and optimizes revenue generation.
9. Population Health Management (PHM) Systems: Integrating EMR systems with PHM systems enables data aggregation, analytics, and reporting for population health initiatives. This integration supports proactive care management, patient stratification, and targeted interventions to improve health outcomes.
10. Interoperability Standards and APIs: Implementing interoperability standards, such as Health Level Seven International (HL7) standards and Fast Healthcare Interoperability Resources (FHIR), and utilizing application programming interfaces (APIs), facilitates the exchange of data between EMR systems and other health IT systems. This promotes seamless data sharing, enhances system connectivity, and fosters innovation.
In summary, integrating electronic medical record systems with other health IT systems, such as LIS, PMS, PACS, HIE, EPCS, telehealth systems, patient portals, RCM systems, PHM systems, and utilizing interoperability standards and APIs, is essential for efficient communication, data exchange, and care coordination. These integrations enhance the functionality and value of EMR systems, resulting in improved patient care, streamlined workflows, and enhanced collaboration among healthcare stakeholders.
Potential Drawbacks of Electronic Medical Record Systems
While electronic medical record (EMR) systems offer numerous benefits, there are also potential drawbacks that healthcare organizations should consider. Understanding these drawbacks helps ensure that the implementation and use of EMR systems are done effectively. Here are some potential drawbacks of electronic medical record systems:
1. Cost and Financial Considerations: Implementing and maintaining an EMR system can be costly, especially for small healthcare organizations with limited resources. The upfront costs include software licensing, hardware infrastructure, training, and ongoing maintenance expenses. Additionally, there may be hidden costs associated with data migration, customization, and system upgrades.
2. Learning Curve and User Training: Adopting an EMR system requires healthcare professionals to learn new technologies, workflows, and documentation methods. The initial learning curve can lead to a temporary decrease in productivity and potentially increase the risk of errors. Adequate user training and ongoing support are necessary to minimize these challenges.
3. Workflow Disruptions: Integrating an EMR system into existing workflows can cause temporary disruptions and changes in established processes. It may take time for healthcare providers and staff to adjust to new workflows and become comfortable with using the system effectively. Proper planning, communication, and training are crucial to mitigate workflow disruptions.
4. Technical Challenges: EMR systems may encounter technical issues, such as system downtime, connectivity problems, or software glitches. These challenges can impact the availability and accessibility of patient information, affecting the quality and timeliness of patient care. Regular maintenance, prompt technical support, and backup systems are necessary to address these technical challenges.
5. Data Security and Privacy Concerns: EMR systems store vast amounts of sensitive patient information, making them potential targets for cyber threats and security breaches. Inadequate security measures, weak passwords, unauthorized access, or malware attacks can compromise the confidentiality and privacy of patient data. Strict security measures, staff training, and compliance with privacy regulations are essential to mitigate security risks.
6. Interoperability Limitations: Achieving seamless interoperability between different EMR systems and health IT systems can be challenging. Incompatibility issues, limited interconnectivity, or differing data standards may hinder the exchange of patient information between healthcare providers. Standardization efforts and adherence to interoperability standards are necessary to address these limitations.
7. Potential for Data Entry Errors: While EMR systems reduce the risk of illegible handwriting, they introduce the possibility of new types of errors. Incorrect data entry, selection of incorrect templates or options, and copying and pasting errors can compromise data accuracy and quality. Implementing proper data validation processes and ongoing quality control measures are necessary to prevent and address these errors.
8. Dependency on Technology: EMR systems rely heavily on technology infrastructure, including computer networks, servers, and software. Any system malfunctions, power outages, or network failures can disrupt access to patient data. Healthcare organizations need to have contingency plans and backup systems in place to ensure continuity of care during technology failures.
9. Documentation Overload: The ease of documentation in EMR systems can lead to an excessive amount of redundant or irrelevant information. This may result in “copy and paste” errors, difficulties in locating critical information, and potential information overload for healthcare professionals. Proper training and the development of documentation best practices can help address these challenges.
10. Loss of Personal Connection: Implementing EMR systems may lead to a perceived loss of personal connection between healthcare providers and patients. Increased focus on computer screens and data entry can create barriers in patient interactions, potentially impacting the quality of patient-provider relationships. Healthcare providers should be mindful of maintaining a balance between technology use and maintaining a personal connection with patients.
In summary, potential drawbacks of electronic medical record systems include cost considerations, learning curve and user training, workflow disruptions, technical challenges, data security and privacy concerns, interoperability limitations, potential data entry errors, dependency on technology, documentation overload, and the perceived loss of personal connection. Balancing these considerations and addressing them proactively can help healthcare organizations optimize the benefits and mitigate the potential drawbacks associated with implementing EMR systems.
Future Trends in Electronic Medical Record Systems
The landscape of electronic medical record (EMR) systems continues to evolve and adapt to the changing needs of the healthcare industry. As technology advances and healthcare practices transform, certain trends are shaping the future of EMR systems. Here are some key future trends in electronic medical record systems:
1. Artificial Intelligence (AI) and Machine Learning: AI and machine learning technologies are being increasingly integrated into EMR systems. These tools can analyze large volumes of healthcare data, automate tasks, make predictions, and provide clinical decision support. AI-driven algorithms can assist in diagnosing diseases, predicting patient outcomes, and identifying treatment options, thereby enhancing healthcare delivery.
2. Interoperability and Health Information Exchange: The push for interoperability continues to grow, and EMR systems are becoming more adept at exchanging patient data seamlessly. Health information exchange networks are expanding, enabling healthcare providers to access comprehensive patient information from various sources, leading to improved care coordination and continuity.
3. Telemedicine Integration: With the rise of telemedicine and virtual care, EMR systems are evolving to integrate with telehealth platforms. This integration allows healthcare providers to document telehealth visits directly into the EMR system, enabling streamlined documentation, billing, and access to visit information. It promotes efficient and effective remote patient care.
4. Mobile Accessibility: EMR systems are increasingly being optimized for mobile devices, such as smartphones and tablets. Mobile apps and responsive web interfaces allow healthcare providers to access patient records, make updates, and perform tasks from anywhere, enhancing flexibility and improving workflow efficiency.
5. Enhanced Patient Engagement: Future EMR systems will focus on enhancing patient engagement and enabling patients to actively participate in their healthcare. This includes features like patient portals, secure messaging, access to personal health records, and health tracking integration. Empowering patients with tools to manage their health fosters better communication and collaboration between patients and healthcare providers.
6. Data Analytics and Population Health Management: EMR systems will increasingly emphasize the use of data analytics for population health management. Advanced analytics tools can leverage EMR data to identify trends, measure outcomes, and monitor population health. This enables healthcare organizations to make data-driven decisions, implement targeted interventions, and improve health outcomes at both individual and population levels.
7. Voice Recognition and Natural Language Processing: The integration of voice recognition and natural language processing capabilities in EMR systems aims to enhance documentation efficiency and accuracy. Voice dictation allows healthcare providers to enter information into the EMR system using spoken commands, reducing the need for manual typing and streamlining the documentation process.
8. Blockchain for Data Security: Blockchain technology holds promise for enhancing data security and integrity in EMR systems. Utilizing blockchain can improve data privacy, ensure secure data sharing, and maintain an immutable record of patient data transactions. This technology has the potential to significantly enhance data security and interoperability in healthcare.
9. Genomics Integration: As genomic medicine advances, EMR systems will evolve to integrate genetic data into patient records. This integration allows healthcare providers to access and interpret genetic information, personalize treatment plans, and improve precision medicine practices.
10. Usability and User Experience: The future of EMR systems will prioritize usability and user experience to enhance healthcare provider satisfaction and workflow efficiency. User-centered design principles will be employed to ensure intuitive interfaces, streamlined processes, and decreased cognitive burden on healthcare professionals.
In summary, future trends in electronic medical record systems include the incorporation of artificial intelligence and machine learning, improved interoperability and health information exchange, integration with telemedicine, mobile accessibility, enhanced patient engagement, data analytics for population health management, voice recognition and natural language processing, blockchain for data security, genomics integration, and a focus on usability and user experience. Embracing these trends will help healthcare organizations leverage technology advancements to deliver more efficient, personalized, and patient-centered care with EMR systems at the forefront.