Early Development of Electronic Medical Records
Electronic Medical Records (EMRs) have revolutionized the healthcare industry, providing a more efficient and streamlined approach to patient care. The journey towards the development and implementation of EMRs can be traced back to the early 1950s. During this time, computers were starting to emerge as powerful tools with the potential to revolutionize data management.
One of the earliest pioneers in the field of electronic medical records was Dr. Larry Weed. In 1955, Dr. Weed proposed the idea of a problem-oriented medical record (POMR) system, which aimed to organize patient data according to specific medical problems. This concept laid the foundation for the future development of EMRs.
In the 1960s, a breakthrough was made with the invention of the computerized patient record system (CPRS). This system, developed at the Massachusetts General Hospital, allowed medical records to be stored electronically, replacing the laborious manual process of paper-based records. CPRS enabled healthcare professionals to access patient data more quickly and efficiently, improving the overall quality of care.
The 1970s saw the rise of the personal computer, which further accelerated the development of electronic medical records. Unlike the large mainframe computers of the past, personal computers were smaller, more affordable, and accessible to individual healthcare providers. This led to the emergence of electronic medical record systems designed specifically for individual practices.
In the 1990s, the concept of electronic health records (EHRs) began to gain attention. EHRs aimed to encompass a broader range of healthcare data beyond the traditional medical record. The goal was to create a comprehensive digital record that could be shared among different healthcare providers, improving communication and coordination of care.
The federal government recognized the potential benefits of electronic medical records and took steps to promote their adoption. In 2004, President George W. Bush set a goal for all Americans to have access to electronic health records by 2014. This initiative led to the establishment of the Office of the National Coordinator for Health Information Technology (ONC) and the widespread implementation of EMR systems.
Advancements in technology have played a significant role in shaping the evolution of electronic medical records. The transition from standalone computer systems to web-based and cloud-based platforms has made EMRs more accessible and scalable. Integration with other healthcare technologies, such as telemedicine and wearable devices, has further expanded the capabilities of EMR systems.
Today, electronic medical records have become an essential tool in modern healthcare, facilitating efficient data management, improving patient outcomes, and enabling better collaboration among healthcare providers. The future holds even more promise for EMRs, with the potential for artificial intelligence and machine learning to further enhance data analysis and decision-making in patient care.
The Birth of the Computerized Patient Record System
In the 1960s, revolutionary advancements in computer technology paved the way for the birth of the Computerized Patient Record System (CPRS). This groundbreaking system transformed the way healthcare providers managed and accessed patient medical records.
The development of the CPRS can be attributed to the collaboration between medical professionals and computer scientists. Their shared vision was to create a more efficient and reliable method of storing and retrieving patient information.
Prior to the CPRS, patient records were predominantly paper-based, resulting in a cumbersome and time-consuming process. Healthcare providers had to manually search through stacks of paper documents to find the necessary information, leading to delays in diagnosis and treatment.
Recognizing these inefficiencies, researchers at the Massachusetts General Hospital, led by Dr. Larry Weed, set out to revolutionize the medical record-keeping system. In 1965, they introduced the Problem-Oriented Medical Information System (PROMIS), considered the precursor to the CPRS.
PROMIS introduced the concept of organizing patient data based on specific medical problems. This problem-oriented approach made it easier for healthcare professionals to navigate through patient records, streamlining the information retrieval process.
Building upon the success of PROMIS, researchers at the Massachusetts General Hospital went on to develop the Computerized Patient Record System in the late 1960s. The CPRS allowed medical records to be stored electronically, replacing the laborious manual process of paper-based records.
The CPRS utilized mainframe computers, which were large and expensive, to store and manage patient data. This marked a significant shift in how healthcare providers accessed and documented patient information.
With the CPRS, healthcare professionals could input and retrieve patient data with just a few keystrokes, saving valuable time and improving the overall efficiency of healthcare delivery. It also eliminated the risks associated with lost or misplaced paper records, ensuring that patient data was secure and readily accessible.
The introduction of the CPRS sparked further advancements in computer technology. As computers became smaller, more affordable, and accessible, the transition from mainframe computers to personal computers was made possible.
This transition opened up new possibilities for the widespread adoption of electronic medical record systems. Individual healthcare practices could now afford to implement their own computerized patient record systems, further streamlining administrative tasks and improving patient care.
The Rise of the Personal Computer in Healthcare
The emergence and widespread adoption of personal computers in the healthcare industry in the 1970s marked a significant milestone in the development of electronic medical records. The rise of personal computers revolutionized data management and transformed the way healthcare professionals interacted with patient information.
Unlike the large mainframe computers of the past, personal computers were smaller, more affordable, and accessible to individual healthcare providers. This newfound accessibility allowed healthcare professionals to have their own dedicated computer systems, enabling them to store and access patient data more conveniently.
With the adoption of personal computers, the healthcare industry witnessed the development of electronic medical record systems specifically designed for use in individual practices. These systems provided a range of functionalities, including patient demographics, medical history, laboratory results, and medication records.
The transition to electronic medical records on personal computers brought numerous benefits to healthcare providers. It streamlined administrative tasks, such as appointment scheduling, billing, and insurance claims processing, allowing healthcare professionals to focus more on patient care.
By digitizing patient records, personal computers enabled healthcare professionals to access and share information quickly and easily. This facilitated better communication and collaboration among different healthcare providers involved in a patient’s care, leading to improved coordination and more accurate decision-making.
Moreover, the use of personal computers in healthcare brought about increased efficiency and accuracy in data entry and storage. Manual paper-based processes were prone to errors and could be time-consuming. With electronic medical record systems, healthcare professionals could input and retrieve patient data with greater speed and accuracy.
The rise of personal computers also played a crucial role in facilitating research and data analysis in healthcare. Researchers could now utilize computer software and statistical tools to analyze large sets of patient data, enabling them to identify trends, patterns, and correlations that could contribute to advancing medical knowledge and improving patient outcomes.
As technology continued to evolve, personal computers became faster, more powerful, and more interconnected. The connectivity allowed for the sharing of electronic medical records across different healthcare facilities and improved interoperability among various systems.
Overall, the rise of personal computers in healthcare revolutionized the way electronic medical records were managed and ushered in a new era of efficiency and convenience. It paved the way for further advancements in technology and set the stage for the development and adoption of more sophisticated electronic health record systems in the years to come.
The Advent of Electronic Health Records
In the 1990s, the concept of Electronic Health Records (EHRs) emerged, marking a crucial turning point in healthcare data management. EHRs represented a shift towards a more comprehensive and interconnected approach to managing patient information.
Unlike traditional electronic medical records (EMRs) that primarily focused on medical and clinical information, EHRs aimed to encompass a broader range of health-related data. This included not only medical records but also information from other healthcare providers, insurance companies, pharmacies, and even patient-generated data.
The advent of EHRs was driven by the need for a more holistic view of a patient’s health, enabling healthcare providers to make more informed decisions and provide better-coordinated care. By consolidating a patient’s medical history, allergies, medications, and other vital information, EHRs fostered improved communication and collaboration among healthcare professionals.
The development of EHR systems paved the way for seamless information exchange among different healthcare settings. With EHRs, healthcare providers could readily access a patient’s records regardless of where they received care, eliminating the need for physical transfer of paper records between institutions.
Another significant aspect of EHRs was the inclusion of computerized physician order entry (CPOE) systems. CPOE systems allowed healthcare providers to enter orders for medications, tests, and procedures electronically, reducing the chances of errors commonly associated with handwritten or verbally communicated orders.
EHRs also introduced features such as decision support tools, which provided healthcare professionals with real-time clinical guidelines and alerts based on a patient’s data. These tools helped improve patient safety and adherence to evidence-based practices by offering valuable insights and reminders during the diagnostic and treatment process.
The adoption of EHRs received significant support from government initiatives and policies. In 2004, then-President George W. Bush set a goal for all Americans to have access to electronic health records by 2014. This led to the establishment of the Office of the National Coordinator for Health Information Technology (ONC), which provided guidance, standards, and financial incentives to encourage the widespread adoption of EHRs.
Today, EHRs have become an indispensable tool in the healthcare industry, streamlining administrative tasks, improving patient safety, and enhancing the overall quality of care. The seamless flow of information facilitated by EHRs allows healthcare providers to make data-driven decisions, resulting in better patient outcomes.
As technology continues to advance, the potential for EHRs to further transform healthcare is immense. With the integration of artificial intelligence, machine learning, and interoperability between different systems, EHRs have the potential to revolutionize disease management, personalized medicine, and population health management.
Federal Support for Electronic Medical Records
The widespread adoption of electronic medical records (EMRs) in the healthcare industry was greatly influenced by the support and initiatives of the federal government. Recognizing the potential benefits of EMRs, the government took steps to promote their use and implementation, with a focus on improving the quality and efficiency of healthcare delivery.
One of the key milestones in federal support for EMRs came in 2004. President George W. Bush set an ambitious goal for all Americans to have access to electronic health records by 2014. This goal served as a catalyst for the widespread adoption and implementation of EMR systems across healthcare organizations.
To support this goal, the federal government established the Office of the National Coordinator for Health Information Technology (ONC) in 2004. The ONC played a crucial role in promoting the adoption of EMRs by providing guidance, setting standards, and developing certification programs for EMR vendors.
In addition to providing guidance, the federal government also implemented financial incentives to encourage healthcare providers to adopt EMRs. The Health Information Technology for Economic and Clinical Health (HITECH) Act, passed in 2009 as part of the American Recovery and Reinvestment Act, established the Meaningful Use program.
The Meaningful Use program provided financial incentives to eligible healthcare providers who demonstrated the meaningful and effective use of EMRs. These incentives served as a significant motivator for healthcare organizations to invest in EMR systems, as they could potentially receive substantial financial benefits for their implementation efforts.
The federal government’s support for EMRs also extended to the development and implementation of health information exchanges (HIEs). HIEs are networks that enable the exchange of patient health information securely and efficiently between different healthcare providers. This interoperability promotes seamless information sharing, improving care coordination and patient outcomes.
Furthermore, the federal government played an instrumental role in addressing privacy and security concerns associated with EMRs. The Health Insurance Portability and Accountability Act (HIPAA) Privacy and Security Rules set standards for the protection and confidentiality of patient health information, ensuring that EMR systems comply with these regulations.
The federal government’s support for EMRs has had a significant impact on the healthcare industry. Today, the majority of healthcare organizations have implemented EMR systems, enabling them to provide more efficient and coordinated care to their patients.
As technology continues to evolve, the government remains committed to promoting the use of EMRs. Efforts are being made to encourage further interoperability and data sharing between different EMR systems and improve the usability and functionality of these systems to enhance the overall quality of healthcare delivery.
Advancements in Electronic Medical Records Technology
Over the years, advancements in technology have led to significant improvements in electronic medical records (EMRs) systems. These advancements have revolutionized the way healthcare providers capture, store, and utilize patient data, enhancing efficiency, accuracy, and patient care outcomes.
One of the notable advancements in EMR technology is the transition from standalone, local server-based systems to web-based and cloud-based platforms. Web-based EMR systems allow healthcare providers to access patient records from any location with an internet connection, eliminating the need for physical servers and enabling remote collaboration.
Cloud-based EMR solutions offer even more flexibility and scalability, as they leverage the power of off-site servers to store and process data securely. Cloud-based systems provide healthcare organizations with the ability to handle large amounts of data, accommodate multiple users simultaneously, and easily scale their infrastructure as their needs evolve.
The integration of artificial intelligence (AI) and machine learning algorithms into EMR systems has opened up new opportunities for leveraging patient data. AI algorithms can analyze vast amounts of complex data, uncover hidden patterns, and generate valuable insights to aid in diagnosis, treatment planning, and personalized medicine.
AI-powered tools, such as natural language processing (NLP), allow healthcare providers to extract meaningful information from unstructured clinical notes. NLP can analyze free-text narratives, making it possible to mine valuable data that would otherwise remain untapped.
Another key advancement in EMR technology is the integration of data from various sources, such as wearable devices and remote monitoring tools. EMR systems can now collect and incorporate data from patient-generated sources, offering a more comprehensive view of a patient’s health status and facilitating proactive and preventive care.
The rise of application programming interfaces (APIs) has also contributed to the improvement of EMR systems. APIs allow different software applications to communicate and share data seamlessly, enhancing interoperability between different healthcare systems. This interoperability enables healthcare providers to exchange information easily and have a more complete picture of a patient’s medical history.
Furthermore, advancements in data analytics have enabled healthcare organizations to derive meaningful insights from large data sets. EMR systems can now generate real-time analytics dashboards and reports, providing healthcare providers with up-to-date information on patient outcomes, population health trends, and quality improvement initiatives.
Usability and user experience have been areas of focus in modern EMR systems. User-centered design principles aim to simplify the user interface, making EMR systems more intuitive and user-friendly. These improvements reduce the learning curve for healthcare providers and allow them to navigate the system more efficiently, ultimately saving time and enhancing patient care.
As technology continues to evolve, so too will EMR systems. Advancements such as blockchain technology, virtual reality, and interoperability standards, like FHIR (Fast Healthcare Interoperability Resources), have the potential to further transform the way patient data is managed, shared, and utilized, leading to even more significant improvements in healthcare delivery.
Current State of Electronic Medical Records
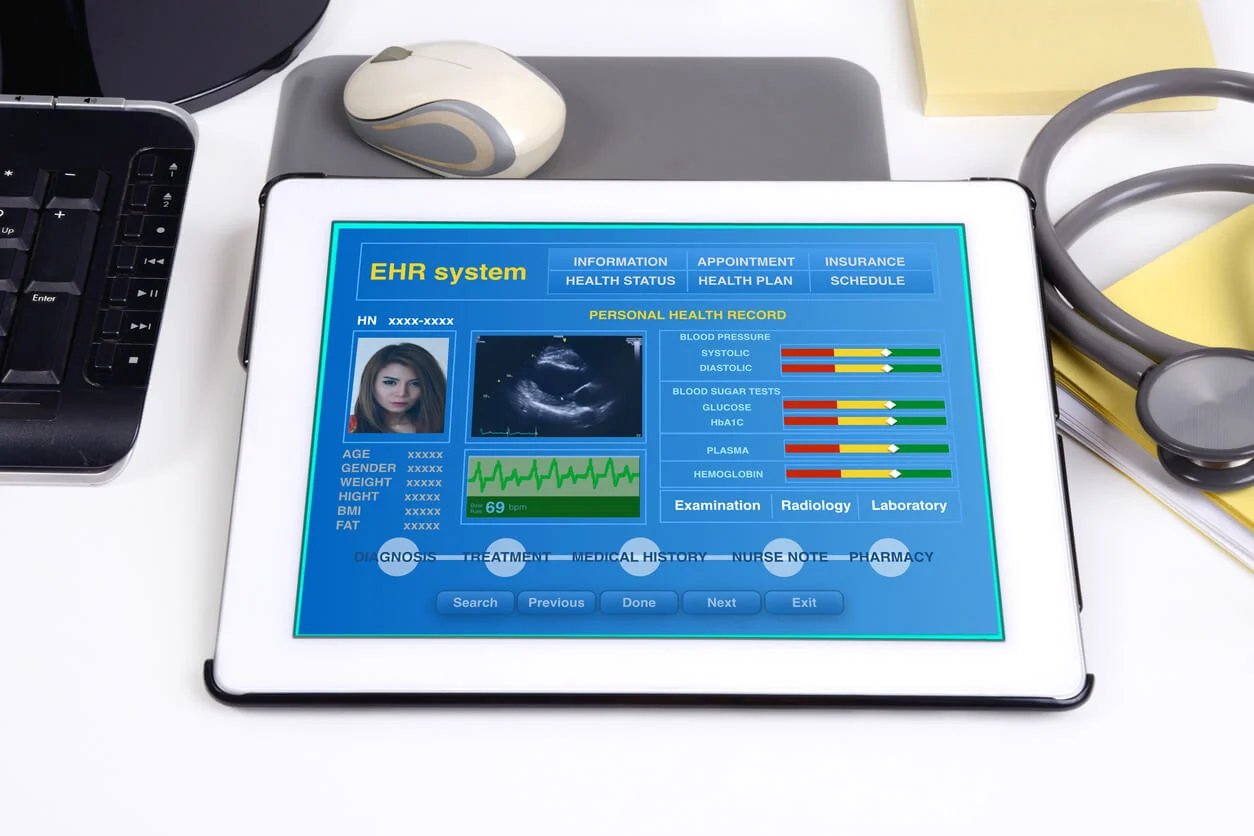
The current state of electronic medical records (EMRs) reflects a significant transformation in healthcare data management. EMRs have become an integral part of modern healthcare, with widespread adoption across healthcare organizations and integration into various aspects of patient care.
Today, the majority of healthcare providers have transitioned from paper-based records to electronic systems. EMRs provide a centralized repository for patient data, including medical history, medications, allergies, laboratory results, and imaging reports.
One of the key features of EMRs is the ability to improve the efficiency and accuracy of clinical documentation. Healthcare providers can enter and access patient information electronically, eliminating the need for deciphering illegible handwriting or searching through stacks of paper records.
EMRs also empower healthcare professionals with enhanced decision-making tools. Clinical decision support systems built into EMRs provide real-time alerts, reminders, and evidence-based guidelines, assisting healthcare providers in making informed choices for diagnosis, treatment, and medication management.
Interoperability is another crucial aspect of the current state of EMRs. The exchange of health information between different healthcare settings is now more feasible, allowing for seamless coordinated care. Health information exchanges (HIEs) and standards like HL7 (Health Level 7) facilitate the secure exchange of patient data, enhancing care coordination and continuity.
Furthermore, advancements in technology have led to the integration of other healthcare systems with EMRs. Picture Archiving and Communication Systems (PACS) allow for the storage and retrieval of medical images directly from EMRs, eliminating the need for physical film records. Integration with pharmacy systems streamlines medication ordering and tracking, reducing medication errors and enhancing patient safety.
Mobile access to EMRs has also become more prevalent in the current state of healthcare. With the proliferation of smartphones and tablets, healthcare providers can now access patient information and input data on-the-go, improving efficiency and allowing for more timely and accurate documentation.
However, challenges persist in the current state of EMRs. One significant challenge is the issue of data privacy and security. As EMRs contain sensitive patient information, strict protocols need to be in place to protect against breaches and unauthorized access. Striking a balance between data security and data accessibility remains an ongoing concern.
Another challenge is the variability in the design and usability of EMR systems. While efforts have been made to improve user interfaces and enhance user experience, there is still room for standardization and optimization to ensure a seamless and intuitive workflow for healthcare providers.
The current state of EMRs also highlights the need for ongoing training and education for healthcare professionals. Continuous training programs are essential to ensure that healthcare providers have the necessary skills to effectively utilize EMR systems and leverage their capabilities for improved patient care.
The Future of Electronic Medical Records
The future of electronic medical records (EMRs) holds immense potential for transforming healthcare delivery and improving patient outcomes. Rapid advancements in technology are paving the way for innovative developments in EMR systems, which will amplify the benefits and capabilities of these electronic platforms.
One significant aspect of the future of EMRs is the integration of artificial intelligence (AI) and machine learning (ML) algorithms. AI-powered EMR systems will have the ability to analyze large volumes of patient data, identify patterns and trends, and generate meaningful insights in real-time. This will assist healthcare providers in making more accurate diagnoses, predicting disease progression, and developing personalized treatment plans.
The incorporation of natural language processing (NLP) will further enhance the capabilities of EMR systems. NLP can extract and analyze unstructured data, such as clinical notes and patient narratives, enabling EMRs to capture a more comprehensive picture of a patient’s health and facilitate more context-aware decision-making by healthcare providers.
The future of EMRs also emphasizes the importance of interoperability and data exchange. Efforts are being made to establish standardized systems and protocols that facilitate seamless information sharing between different EMR platforms. This interoperability will allow healthcare providers to access and utilize patient data from various sources, leading to more comprehensive and coordinated care.
Emerging technologies, such as blockchain, have the potential to revolutionize the security and integrity of patient data within EMRs. Blockchain can provide a decentralized and tamper-proof system for storing and sharing health information, ensuring patient privacy while enabling secure data exchange and accessibility.
Another area of growth in the future of EMRs is the integration of telehealth and remote patient monitoring. EMR systems will incorporate features that allow healthcare providers to remotely monitor patient vitals and collect data from wearable devices. This provides opportunities for more personalized and proactive care, allowing healthcare providers to intervene early and offer timely interventions.
As technology continues to advance, the user experience of EMR systems will also undergo significant improvements. User-centered design principles will shape the development of intuitive and user-friendly interfaces, reducing the burden on healthcare providers and enhancing workflow efficiency.
Additionally, the future of EMRs will see an increased focus on patient engagement and empowerment. EMR systems will evolve to provide patients with access to their own records, enabling them to actively participate in their healthcare decisions and improve self-management of chronic conditions.
Big data analytics will play a vital role in the future of EMRs. The vast amount of data generated by EMR systems will be leveraged to identify population health trends, develop predictive models for disease outbreaks, and refine treatment protocols to improve overall healthcare outcomes at a population level.