Electrode Placement for Monitoring Contractions
Monitoring uterine contractions is an essential part of assessing labor progress in pregnant individuals. To accurately monitor contractions, electrodes are placed on the abdomen to detect the electrical activity of the uterus. Proper electrode placement is crucial for obtaining accurate readings and ensuring an effective monitoring process.
When positioning the electrodes, it’s important to consider the placement relative to the uterine muscle fibers. Typically, two electrodes are used: one above the umbilicus and the other below. Placement above the umbilicus ensures that the uterine fundus is monitored, while placement below allows for monitoring of the lower segment. The electrodes should be positioned in a way that maximizes contact with the skin surface and avoids any interference from other objects.
Before placing the electrodes, it’s vital to clean the skin surface thoroughly. This helps eliminate any oils or dirt that could interfere with the electrode’s adhesive properties. Additionally, the use of conductive gel can enhance the electrical connectivity between the electrode and the skin.
When applying the electrodes, ensure that the adhesive surface is properly aligned with the marked placement areas. Firmly press the electrodes onto the skin to ensure good contact and optimal signal transmission. Avoid excessive tension on the electrode wires, as it can cause discomfort for the individual and potentially displace the electrodes.
Regular inspection of the electrodes is necessary to monitor their integrity and ensure continued optimal performance. If an electrode becomes loose, reposition it immediately to maintain a reliable signal. Monitoring staff should also be vigilant for any signs of skin irritation or discomfort, and take appropriate action if needed.
Overall, correct electrode placement is vital for accurate monitoring of uterine contractions during labor. By diligently following proper placement techniques and regularly checking the electrodes, healthcare providers can ensure reliable and informative data that can assist in identifying any abnormal contractions and monitoring labor progression effectively.
Identifying Uterine Contractions on a Monitor
Monitoring uterine contractions is a key component of evaluating labor progress. The ability to accurately identify contractions on a monitor is crucial for healthcare providers to assess the effectiveness of labor and make informed decisions regarding patient care.
When observing a monitor tracing, uterine contractions appear as regular, rhythmic waves. These waves are represented by an increase in the height and frequency of the tracing. Typically, contractions are measured in millimeters of mercury (mmHg) or Montevideo units (MVUs).
During contractions, the uterine muscles contract and exert pressure on the fetus. This pressure generates the characteristic wave pattern on the monitor. The amplitude of the contraction represents the intensity or strength of the uterine muscle contraction. Higher amplitude indicates stronger contractions, while lower amplitude suggests weaker contractions.
Additionally, the duration of a contraction is an essential aspect of monitoring. The duration is measured from the start of the contraction until its completion. Healthy contractions usually last between 30 and 60 seconds. Prolonged contractions that exceed 90 seconds may indicate potential issues and require further evaluation.
Another crucial factor in identifying contractions on a monitor is the frequency of the contractions. Contractions are measured by the time interval between the start of one contraction and the start of the next. In normal labor, contractions occur approximately every 2 to 3 minutes, but this can vary between individuals.
It’s important to note that movements other than contractions, such as fetal activity, maternal movement, or external pressure, can produce artifacts on the monitor tracing. These artifacts can sometimes be mistaken for uterine contractions. Therefore, it’s essential to carefully assess the pattern and characteristics of the waves to differentiate between true contractions and other movements.
When monitoring contractions, providers should also be familiar with the variations in contraction patterns. For example, irregular contractions may indicate early labor, while regular contractions suggest active labor. Additionally, variations in the height and duration of contractions can provide valuable insights into labor progression.
Differentiating Uterine Contractions from Other Movements
When monitoring uterine contractions, it is essential to distinguish them from other movements that may appear on the monitoring tracing. Accurate identification ensures that healthcare providers can make informed decisions regarding labor progress and patient care.
One common movement that may be mistaken for uterine contractions is fetal activity. Fetal movements, such as kicks, rolls, and hiccups, can create temporary disruptions in the monitoring tracing. However, these movements tend to be irregular and do not exhibit the characteristic pattern of uterine contractions. Such movements are typically shorter in duration and have a lower amplitude compared to contractions.
Maternal movements can also cause artifacts on the monitoring tracing and be mistakenly identified as contractions. These movements can include shifting positions, coughing, sneezing, or even talking. It’s important for healthcare providers to familiarize themselves with the typical patterns and characteristics of maternal movements to differentiate them from true contractions.
External pressure can also generate false signals on the monitoring tracing. This pressure can occur when the patient is leaning against or being pressed by external objects, such as a bed railing or an IV pole. These artifacts can mimic the appearance of a contraction, but they lack the regularity and intensity typically seen with uterine contractions.
To accurately differentiate uterine contractions from other movements, healthcare providers should observe the pattern and characteristics of the tracing. Uterine contractions typically exhibit a rhythmic and repetitive pattern, with a gradual increase in height and frequency. The duration and amplitude of contractions are also key indicators.
One useful technique for differentiating contractions from other movements is the palpation of the uterine fundus. By placing a hand on the patient’s abdomen and feeling the contractions while simultaneously monitoring the tracing, healthcare providers can correlate the observed movement with the pattern on the monitor.
It’s important for healthcare providers to communicate and collaborate with the patient to gather additional information. The patient can provide valuable insights into their perception of contractions and movements, helping to validate the accuracy of the monitor tracing.
Overall, careful observation of the pattern, duration, amplitude, and correlation with palpation can aid in differentiating uterine contractions from other movements. Healthcare providers should be vigilant and familiar with the characteristics of both to ensure accurate monitoring and appropriate decision-making during labor.
How to Measure the Intensity of a Contraction
Measuring the intensity of uterine contractions is important for assessing the progress of labor and evaluating the effectiveness of the contractions. There are several methods used to quantify and measure the intensity of contractions, providing healthcare providers with valuable information for patient care decisions.
One commonly used method to measure the intensity of a contraction is by assessing the amplitude of the contractions on the monitoring tracing. The amplitude refers to the height of the contracting wave. It is measured in millimeters of mercury (mmHg) or Montevideo units (MVUs). Higher amplitudes indicate stronger contractions, while lower amplitudes suggest weaker contractions.
In addition to assessing the amplitude, healthcare providers may use subjective measures reported by the patient to estimate the intensity of contractions. The patient can provide feedback on their level of discomfort or pain during contractions, using a pain scale or describing their experience as mild, moderate, or intense. This subjective measure can give valuable insights into the impact of contractions on the patient’s overall experience.
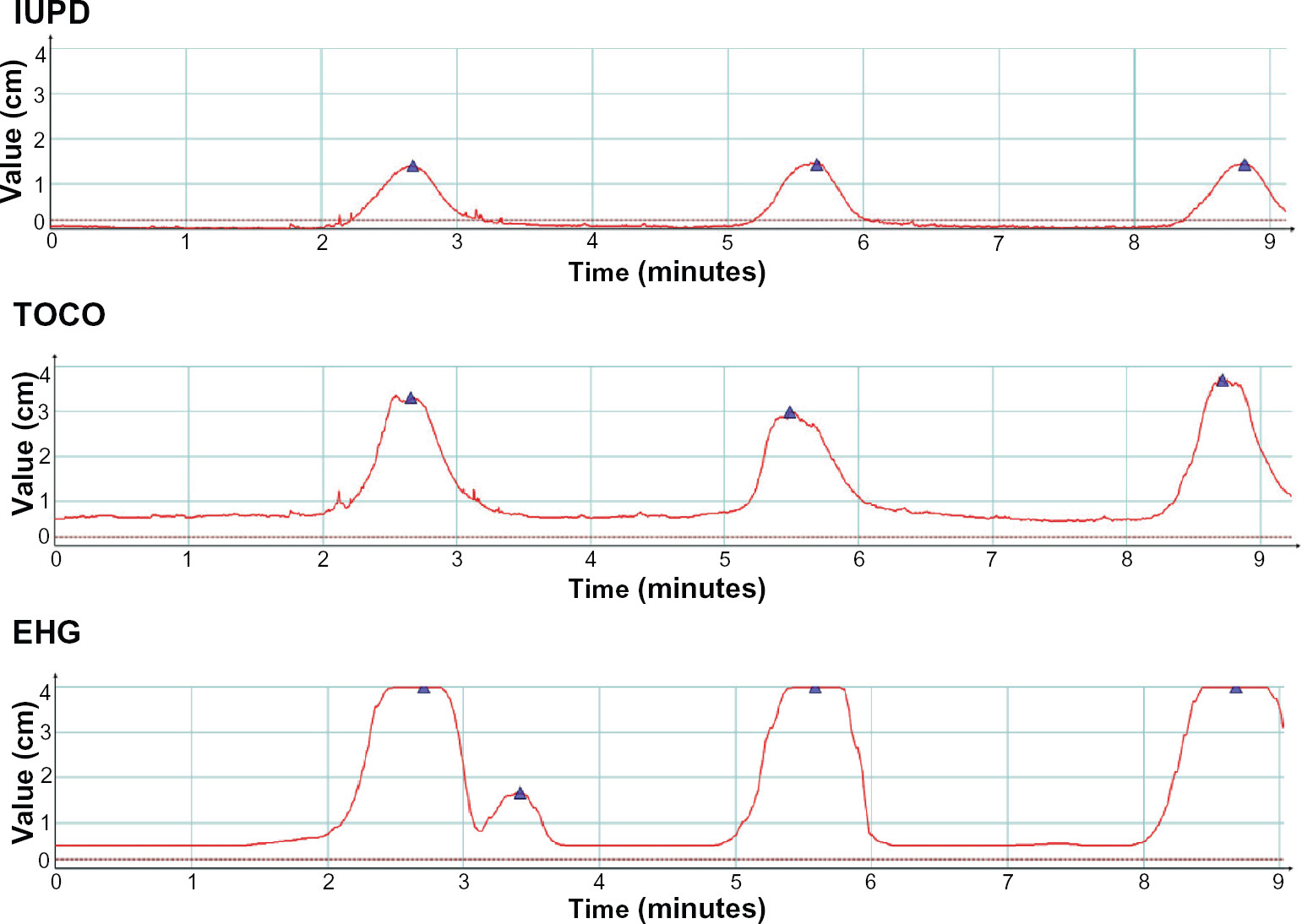
Another method that can provide an objective measurement of contraction intensity is through the use of an intrauterine pressure catheter (IUPC). An IUPC is inserted into the uterine cavity and measures the pressure inside the uterus during contractions. This measurement provides a more accurate and direct assessment of the force exerted by the uterine contractions.
Healthcare providers can also assess the intensity of a contraction by evaluating the level of palpable tension or firmness in the uterine muscles. By placing their hand on the patient’s abdomen and palpating the uterine fundus during a contraction, providers can estimate the intensity based on the level of resistance to their touch.
It’s important to note that the intensity of contractions can vary greatly between individuals and even within the same individual during different stages of labor. Factors such as the position of the baby, maternal factors, and the progression of labor can all influence the intensity of contractions.
By utilizing a combination of objective measurements, subjective reports from the patient, and clinical assessment techniques, healthcare providers can gain a comprehensive understanding of the intensity of contractions. This information allows for more informed decision-making regarding pain management, the progression of labor, and potential interventions to enhance labor progress.
Understanding the Duration of a Contraction
The duration of uterine contractions plays a crucial role in assessing labor progress and monitoring the effectiveness of contractions. Understanding the duration of contractions provides healthcare providers with valuable information to make informed decisions about patient care during labor.
The duration of a contraction is measured from the start of the contraction until its completion. Typically, healthy contractions last between 30 and 60 seconds. However, the duration can vary between individuals and throughout different stages of labor.
Prolonged contractions that exceed 90 seconds may indicate potential issues and require further evaluation. These long-lasting contractions can be associated with decreased blood flow to the placenta and may require intervention to alleviate any potential complications.
It’s important to note that the duration of contractions can fluctuate throughout labor. During the early stages of labor, contractions may be shorter in duration and less intense. As labor progresses, the duration of contractions usually increases, indicating the active phase of labor.
Monitoring the duration of contractions is essential for healthcare providers to assess labor progress accurately. Consistently shorter contractions may suggest inadequate uterine activity, while excessively long contractions may cause fatigue and hinder effective labor progression.
Healthcare providers can assess the duration of contractions by carefully observing the timing of the start and end of each contraction on the monitor tracing. They may also use palpation techniques on the patient’s abdomen to feel the duration of the contraction.
Tracking the duration of contractions over time allows healthcare providers to identify any changes or trends. If contractions consistently become shorter and less effective, it may indicate the need for interventions to augment labor, such as administering oxytocin or changing the patient’s position.
Understanding the duration of contractions is crucial for ensuring a safe and successful labor experience. By closely monitoring contraction duration and recognizing any deviations from the norm, healthcare providers can make timely and informed decisions to optimize labor progress and ensure the well-being of both the mother and baby.
Monitoring the Frequency of Uterine Contractions
Monitoring the frequency of uterine contractions is an essential component of assessing labor progress and determining the effectiveness of contractions. By closely monitoring contraction frequency, healthcare providers can gather valuable information to make informed decisions regarding patient care during labor.
The frequency of contractions is measured by the time interval between the start of one contraction and the start of the next. In normal labor, contractions typically occur approximately every 2 to 3 minutes. However, it’s important to note that the frequency of contractions can vary between individuals and throughout different stages of labor.
Monitoring the frequency of contractions helps healthcare providers evaluate the progression of labor accurately. Consistently irregular contractions or contractions that are too infrequent may suggest labor is not progressing optimally. Conversely, excessively frequent contractions may signal potential complications and require closer monitoring.
Healthcare providers typically rely on several methods to monitor the frequency of contractions. The most common method is through observation of the monitor tracing, which displays the start and end times of each contraction. This provides a visual representation that allows for precise measurement of the time interval between contractions.
In addition to the monitor tracing, healthcare providers may also use palpation techniques to assess the frequency of contractions. By placing their hand on the patient’s abdomen and feeling the onset of each contraction, they can estimate the time interval between contractions.
Monitoring the frequency of contractions throughout labor allows healthcare providers to identify any changes or trends. If contractions become more frequent, it may indicate a progression into the active phase of labor. Conversely, a decrease in the frequency of contractions may call for interventions to augment labor, such as administering oxytocin or recommending position changes.
Regular monitoring of the contraction frequency also helps evaluate the effectiveness of interventions aimed at regulating and improving contractions. For example, if medication is administered to strengthen contractions, monitoring the frequency provides immediate feedback on the intervention’s impact.
By closely monitoring the frequency of contractions, healthcare providers can gain valuable insights into labor progress and make informed decisions about patient care. Effective monitoring ensures timely interventions and promotes optimal outcomes for both the mother and baby.
Variations in Contraction Patterns
Contractions during labor can exhibit various patterns, and understanding these variations is crucial for healthcare providers to accurately assess labor progress and make informed decisions regarding patient care. By closely monitoring and recognizing different contraction patterns, providers can identify any deviations from the normal progression of labor.
One common variation in contraction patterns is irregular or sporadic contractions. These contractions occur unpredictably and do not follow a regular pattern of increasing frequency or intensity. Irregular contractions are often observed during the early phase of labor and are considered a normal part of the preparatory process.
On the other hand, regular contractions follow a predictable pattern with consistent frequency and intensity. Regular contractions are typically observed during the active phase of labor, indicating progressive cervical dilation and effacement.
Another variation is the occurrence of hypertonic or “too frequent” contractions. These contractions are characterized by their increased frequency, occurring closer together than the usual 2 to 3 minute interval. Hypertonic contractions can lead to inadequate relaxation and blood flow, potentially causing distress for the baby and fatigue for the mother.
Conversely, hypotonic or “too weak” contractions are characterized by their decreased intensity and duration. Hypotonic contractions may be insufficient to effectively dilate the cervix and progress labor. In such cases, interventions such as artificial rupture of membranes or administration of oxytocin may be considered to stimulate stronger contractions.
Some individuals may experience a double-peak or multiple-peak contraction pattern. This pattern is characterized by two or more distinct peaks within a single contraction. Double-peak contractions can prolong the labor process and may require careful monitoring for any associated complications.
Occasionally, individuals may experience what is known as the ring of fire, a sensation of intense burning and pressure in the vaginal area during the descent of the baby. This sensation is often accompanied by a temporary pause or plateau in contractions, allowing the perineum to stretch and accommodate the passage of the baby’s head.
It’s important for healthcare providers to closely monitor and document any variations in contraction patterns throughout labor. Continuous assessment allows providers to identify potential issues early and make adjustments to ensure optimal labor progress and minimize any associated risks.
By recognizing and understanding the various variations in contraction patterns, healthcare providers can provide appropriate support and interventions to optimize labor outcomes and ensure the well-being of both the mother and the baby.
Interpreting Contraction Tracings
Interpreting contraction tracings is a vital skill for healthcare providers to evaluate labor progress and ensure the well-being of both the mother and the baby. Contraction tracings, also known as uterine monitoring tracings, provide valuable information about the frequency, intensity, and duration of contractions.
When interpreting contraction tracings, healthcare providers examine several key factors. The first aspect to consider is the baseline or resting tone of the uterus. The baseline represents the level of uterine activity between contractions. A normal resting tone falls within the range of 10 to 20 mmHg or Montevideo units (MVUs). Deviations from this range may indicate uterine hyperactivity or inadequate resting tone.
Another crucial element in interpreting contraction tracings is the amplitude or height of each contraction. This measurement indicates the intensity or strength of uterine contractions. Higher amplitudes reflect stronger contractions, while lower amplitudes suggest weaker contractions. Comparing the amplitude of contractions throughout labor helps monitor changes and assess labor progression.
Healthcare providers also analyze the duration of contractions on the tracing. Duration is measured from the beginning to the end of a contraction. The normal duration of a contraction typically ranges between 30 and 60 seconds. Prolonged contractions exceeding 90 seconds may indicate issues such as uterine hyperstimulation or compromised blood flow to the placenta.
Additionally, the frequency of contractions is a significant factor in interpretation. Frequency represents the time interval between the start of one contraction and the start of the next. In a normal labor, contractions occur approximately every 2 to 3 minutes. Deviations from this range may indicate labor abnormalities or the need for intervention.
When interpreting contraction tracings, healthcare providers also consider the overall pattern of contractions. Regular, progressive contractions reflect effective labor progression. Irregular patterns may suggest early labor or other factors affecting labor progression. Variations in contraction patterns, such as hypertonic or hypotonic contractions, require close monitoring and potential intervention.
It is crucial for providers to differentiate uterine contractions from other movements on the tracing. Fetal movements, maternal movements, or external pressures can create artifacts that may be mistaken for contractions. Close examination of the pattern, timing, and characteristics can help distinguish true contractions from other movements on the tracing.
In addition to the visual interpretation, healthcare providers can use available software or tools to measure and document key parameters of the contractions. These measurements can aid in accurate assessment, comparison, and documentation of contractions throughout labor.
By carefully interpreting contraction tracings, healthcare providers gain valuable insights into uterine activity and labor progress. Effective interpretation guides decision-making, facilitates appropriate interventions, and promotes optimal outcomes for both the mother and the baby.
Significance of Early versus Late Decelerations during Contractions
Decelerations during contractions are important indicators of fetal well-being and can provide healthcare providers with valuable information about the status of the baby. Two types of decelerations commonly observed during contractions are early and late decelerations. Understanding the significance of early and late decelerations is crucial for healthcare providers to intervene promptly and ensure the safety of the baby.
Early decelerations are usually benign and occur as a result of fetal head compression during contractions. These decelerations typically mirror the shape and duration of the contraction. They are characterized by a gradual decrease in the fetal heart rate (FHR) coinciding with the start of the contraction and a return to the baseline as the contraction ends.
Early decelerations are generally considered reassuring and reflective of a well-oxygenated baby. They typically do not require immediate intervention and are closely associated with normal labor progression. However, ongoing monitoring is necessary to ensure that the pattern remains consistent and that there are no additional signs of fetal distress.
On the other hand, late decelerations are concerning and may indicate compromised fetal oxygenation. Late decelerations are characterized by a delayed drop in the FHR, occurring after the peak of the contraction. The FHR returns to the baseline after the contraction ends. The presence of late decelerations suggests inadequate blood flow and oxygen supply to the baby.
Late decelerations can be caused by various factors, including uteroplacental insufficiency, maternal hypotension, or placental abnormalities. These decelerations require immediate attention and may necessitate interventions to optimize fetal oxygenation. Healthcare providers often recommend changing the maternal position, administering intravenous fluids, or considering oxygen supplementation to improve blood flow to the baby.
Differentiating between early and late decelerations is crucial, as their management and implications differ significantly. Early decelerations are considered reassuring and do not require immediate intervention, while late decelerations indicate potential fetal distress and necessitate immediate action.
Continuous monitoring of the FHR and observation of the deceleration patterns during contractions are essential in identifying early or late decelerations. Healthcare providers must be diligent in recognizing signs of potential fetal distress, as timely intervention can significantly impact the outcome for both the mother and the baby.
Overall, the significance of early versus late decelerations during contractions lies in their implications for fetal well-being. Early decelerations are generally benign, reflecting normal labor progress, while late decelerations indicate compromised fetal oxygenation and require immediate attention. Healthcare providers must closely monitor and interpret deceleration patterns to ensure timely intervention and optimize the safety and well-being of the baby.
Monitoring Contraction Progress during Labor
Monitoring the progress of contractions is a critical aspect of assessing labor and ensuring the effective progression of labor. By closely monitoring the frequency, intensity, duration, and pattern of contractions, healthcare providers can make informed decisions regarding patient care and interventions during labor.
One key aspect to monitor is the frequency of contractions. The interval between contractions is an important indicator of labor progress. Typically, contractions occur every 2 to 3 minutes during active labor. Monitoring the regularity and consistency of contractions allows healthcare providers to assess whether labor is progressing steadily or if interventions may be necessary to stimulate contractions.
The intensity of contractions is another crucial parameter to monitor. The strength of a contraction reflects the effectiveness of uterine contractions in promoting cervical dilation and fetal descent. Healthcare providers may use visual observation, palpation, or monitoring devices to assess the intensity of contractions. Monitoring the intensity allows providers to determine if contractions are sufficiently strong to facilitate labor progression or if interventions are needed to augment the strength of contractions.
The duration of contractions is also an important factor to monitor. The average duration of a contraction is between 30 and 60 seconds. Prolonged contractions that exceed 90 seconds may indicate complications and the need for further evaluation. Monitoring the duration of contractions helps assess the efficiency of uterine contractions and the progress of labor.
In addition to frequency, intensity, and duration, healthcare providers should closely monitor the pattern of contractions. Regular, rhythmic contractions with predictable patterns indicate effective labor progress. Irregular or erratic contractions may require closer monitoring and evaluation to determine the underlying cause and appropriate interventions.
Monitoring the progress of contractions is typically done through continuous electronic fetal monitoring (EFM). EFM allows for real-time monitoring of contractions and provides a visual representation of their frequency and intensity. Additional tools, such as uterine pressure catheters, may be used to provide a more accurate measurement of intrauterine pressure and contraction intensity.
Regular and thorough monitoring of contractions during labor enables healthcare providers to assess labor progress accurately and make timely decisions regarding patient care. It allows for identification of any deviations from normal patterns, early recognition of potential complications, and appropriate interventions to optimize labor outcomes.
Effective monitoring of contraction progress requires a combination of clinical assessment skills and the use of monitoring technologies. By closely monitoring the frequency, intensity, duration, and pattern of contractions, healthcare providers can ensure the safe and successful progression of labor for both the mother and the baby.
Analyzing the Effectiveness of Contractions in Labor Progression
The effectiveness of contractions plays a crucial role in labor progression. Analyzing the strength, duration, and pattern of contractions provides healthcare providers with vital information about the efficiency of labor and guides decision-making for interventions and patient care.
One key factor in analyzing the effectiveness of contractions is the intensity or strength of each contraction. Strong contractions are essential for promoting cervical dilation and facilitating the descent of the baby through the birth canal. Healthcare providers assess the intensity of contractions through visual observation, palpation, or electronic monitoring. If contractions are consistently weak or do not meet the desired intensity, interventions such as augmentation or medication may be considered to enhance contraction strength.
The duration of contractions is another important aspect to analyze. Contractions that are too short may not provide enough time for effective cervical dilation and fetal descent. Conversely, excessively long contractions can lead to fatigue and compromise uterine blood flow, potentially impacting fetal well-being. Analyzing the duration of contractions helps healthcare providers determine if contractions are of sufficient length to promote labor progression.
Monitoring the pattern of contractions is also crucial in analyzing their effectiveness. Regular, rhythmic contractions with consistent intervals indicate a favorable pattern for labor progression. In contrast, irregular or erratic contractions may impede labor progress and require closer monitoring and potential interventions. Analyzing the pattern of contractions helps ensure that labor is proceeding in a predictable and efficient manner.
Healthcare providers may use additional tools to analyze the effectiveness of contractions. Intrauterine pressure catheters (IUPCs) can provide a more precise measurement of intrauterine pressure during contractions, helping to assess the force and effectiveness of contractions. Combined with electronic fetal monitoring (EFM), which monitors both the fetal heart rate and contractions, healthcare providers gain a comprehensive understanding of labor progress and the impact of contractions on fetal well-being.
Analyzing the effectiveness of contractions requires continuous monitoring and assessment throughout labor. Healthcare providers document the frequency, intensity, duration, and pattern of contractions as labor progresses. Comparing these parameters over time helps identify trends, deviations, or abnormalities in labor progression and guides appropriate actions and interventions.
Effective analysis of contractions’ effectiveness allows healthcare providers to make informed decisions about patient care and interventions to optimize labor progression. By carefully assessing the strength, duration, and pattern of contractions, healthcare providers can support women in achieving a safe and successful labor experience.
Common Misinterpretations of Contraction Patterns
Interpreting contraction patterns during labor is a crucial skill for healthcare providers. However, there are common misinterpretations that can occur, potentially leading to misunderstandings about the progress of labor and unnecessary interventions. It is important to be aware of these misinterpretations and strive for accurate analysis of contraction patterns.
One common misinterpretation is mistaking irregular contractions for abnormal labor progress. During the early stages of labor, contractions can be irregular in frequency and intensity. This irregularity is normal and often referred to as the “latent phase” of labor. Mistaking irregular contractions for active labor can lead to unnecessary interventions and interventions that may hinder the natural progression of labor.
Another misinterpretation is assuming that stronger contractions always indicate better labor progress. While strong contractions are important for cervical dilation, the effectiveness of contractions should be assessed in conjunction with cervical changes and other signs of progress. Strong contractions without significant cervical dilation may suggest cervical “fighting,” where the cervix resists dilation despite intense contractions. This misinterpretation can lead to unnecessary interventions or prematurely labeling labor as dysfunctional.
Conversely, mistaking weak contractions as an indication of labor not progressing can also be misleading. Labor progress should be evaluated holistically, considering factors such as cervical changes, fetal descent, and the overall pattern of contractions. Weak contractions that are still resulting in cervical change may indicate a slower but steady progression of labor. Rushing to intervene based solely on contraction strength can disrupt the natural rhythm of labor.
Another common misinterpretation is assuming that a prolonged resting phase between contractions indicates a stalled labor. Resting phases, where contractions are less frequent or shorter in duration, can be a normal part of labor progression. These resting periods allow for the recovery of the uterus and may even contribute to successful cervical dilation. Misinterpreting resting phases as stalled labor can result in unnecessary interventions or premature augmentation.
Artifacts and technical issues can also lead to misinterpretations of contraction patterns. External factors such as maternal movement, fetal movement, or poor electrode contact can create artifacts that mimic contractions. Misidentifying these artifacts as actual contractions may lead to inaccurate assessments of labor progress and unnecessary interventions.
To mitigate misinterpretations of contraction patterns, healthcare providers should adopt a comprehensive approach that includes assessing multiple factors such as cervical dilation, station, and the overall progress of labor. Regular communication with the laboring woman and integration of her feedback are also essential for accurate interpretation. Striving for a holistic understanding of the labor process helps providers avoid common misinterpretations and fosters a more individualized and supportive approach to care.
The Role of Contraction Monitors in Identifying Preterm Labor
Contraction monitors play a crucial role in the early identification and monitoring of preterm labor. Preterm labor, defined as labor that begins before 37 weeks of gestation, requires timely intervention to reduce the risk of complications for both the mother and baby. Contraction monitors provide valuable data that healthcare providers can use to assess uterine activity and make informed decisions regarding the management of preterm labor.
Contraction monitors detect and record the frequency, duration, and intensity of uterine contractions. By continuously monitoring uterine activity, these devices provide a comprehensive picture of contractions over time, helping healthcare providers identify potential signs of preterm labor.
When monitoring for preterm labor, contraction monitors enable healthcare providers to recognize patterns of uterine activity that may suggest cervical changes and early labor. Regular and significant contractions that occur more frequently than every 10 minutes or are accompanied by cervical changes can indicate the onset of preterm labor.
Contraction monitors also assist in the evaluation of the effectiveness of interventions to prevent preterm labor. For instance, medications such as tocolytics or bed rest may be prescribed to delay labor. By using contraction monitors, healthcare providers can assess the impact of these interventions on uterine activity and make adjustments as needed.
In addition to monitoring uterine contractions, contraction monitors can be used in combination with other diagnostic tools to evaluate cervical changes. Transvaginal ultrasound or digital cervical examination, along with concurrent contraction monitoring, can provide a comprehensive evaluation of preterm labor risk.
Nonetheless, it is essential to note that contractions detected by contraction monitors alone may not definitively confirm or rule out preterm labor. Clinical assessment, maternal symptoms, and additional diagnostic tests are necessary for a comprehensive evaluation.
Another important aspect of contraction monitors is their ability to provide continuous monitoring. This allows healthcare providers to identify changes in uterine activity over time and make real-time decisions regarding further assessment, therapy, or transfer to a specialized facility equipped to manage preterm labor and its potential complications.
Early identification of preterm labor enables healthcare providers to take proactive measures to prevent or manage preterm birth. Interventions such as administration of medications to mature the baby’s lungs, antenatal corticosteroids, or transfer to a neonatal intensive care unit can be facilitated when preterm labor is detected promptly.
Ultimately, contraction monitors serve as valuable tools in the identification and monitoring of preterm labor. By providing continuous monitoring of uterine contractions and assisting in the evaluation of interventions, contraction monitors enable healthcare providers to take appropriate actions to prevent or manage preterm labor, ultimately improving outcomes for both the mother and baby.
Assessing Uterine Activity during Induced Labor
Assessing uterine activity during induced labor is crucial for healthcare providers to ensure that labor progresses effectively and safely. Induced labor is initiated using medical interventions to stimulate contractions when labor fails to start spontaneously or when there are medical concerns that require delivery. Monitoring uterine activity during induced labor allows healthcare providers to closely monitor the progress of labor and make informed decisions regarding the management of labor induction.
Continuous monitoring of uterine activity during induced labor is typically done using contraction monitors. These monitors detect and record the frequency, duration, and intensity of contractions, providing essential data for healthcare providers to assess the effectiveness of the induction process.
Monitoring uterine activity during induced labor helps healthcare providers determine if contractions are occurring frequently and with sufficient intensity to promote cervical dilation and the descent of the baby. It allows for the assessment of the regularity and strength of contractions, as well as the intervals between contractions.
Assessing the frequency of contractions is an important aspect of monitoring induced labor, as it helps providers to ensure that contractions are occurring at an appropriate pace. In most cases, contractions during induced labor should occur every 2 to 3 minutes. Monitoring the frequency of contractions allows providers to recognize any abnormalities or potential issues that may require intervention.
The intensity of contractions is another crucial parameter to assess during induced labor. Strong and effective contractions promote cervical dilation and efficient labor progression. Healthcare providers may use visual observation, palpation, or electronic monitoring to assess contraction intensity. Monitoring the intensity of contractions helps evaluate the effectiveness of the induction process and guides decisions regarding the need for interventions to augment or strengthen contractions, if necessary.
In addition to frequency and intensity, monitoring uterine activity during induced labor enables healthcare providers to assess the pattern of contractions. Regular and rhythmic contractions reflect a favorable pattern for labor progression, whereas irregular or inconsistent contractions can indicate potential issues that require further assessment or intervention.
Continuous monitoring of uterine activity during induced labor allows healthcare providers to identify any deviations from the expected progress, such as tachysystole (excessively frequent contractions), increased uterine activity without effective cervical changes, or inadequate uterine activity with insufficient cervical dilation. These deviations can signal potential complications and guide decisions regarding the need for intervention or adjustment of the induction process.
Overall, assessing uterine activity during induced labor is vital for healthcare providers to monitor the effectiveness of the induction process, ensure safe labor progression, and make informed decisions regarding patient care. Continuous monitoring using contraction monitors allows for real-time assessment and adjustment of interventions to optimize outcomes for both the mother and the baby.
Recording and Documenting Contraction Patterns
Recording and documenting contraction patterns is an essential task in the monitoring of labor progression. Accurate and thorough documentation provides healthcare providers with a comprehensive record of the frequency, duration, intensity, and pattern of contractions, enabling them to monitor labor effectively and make informed decisions regarding patient care.
When recording contraction patterns, healthcare providers typically note the start and end times of each contraction. This information allows for the calculation of the duration of each contraction and the time intervals between contractions, providing important data for assessing labor progress.
The intensity of contractions is also recorded and documented. Providers may use a scale or measurement system, such as millimeters of mercury (mmHg) or Montevideo units (MVUs), to quantify the strength of each contraction. Accurate documentation of contraction intensity helps in evaluating the effectiveness of labor and guiding appropriate interventions.
The frequency of contractions is a critical aspect of documentation. Providers record the time interval between the start of one contraction and the start of the next. This information is crucial for assessing the regularity and consistency of contractions, as well as identifying any abnormal patterns that may require closer monitoring or intervention.
In addition to frequency, duration, and intensity, documenting the pattern of contractions is important. Providers note whether contractions are regular and rhythmic, showing a predictable pattern, or irregular and sporadic. Documenting the pattern helps track any changes, evaluate the progression of labor, and identify potential issues that may require further assessment or intervention.
Healthcare providers may use various methods for recording and documenting contraction patterns. This can include manual charting on paper, electronic charting systems, or specialized software designed for contraction monitoring. Regardless of the method used, it’s essential to ensure clear and accurate documentation, including clear labeling and appropriate annotation of any notable findings or interventions.
Regular and consistent documentation of contraction patterns throughout labor allows for the tracking of trends and changes over time. It provides a historical record that can be referred to for comparisons, analysis, and decision-making during labor management.
Effective communication and collaboration among the healthcare team regarding the recorded contraction patterns are also crucial. Sharing accurate and updated information helps ensure consistent monitoring and coordinated care for the laboring individual.
By diligently recording and documenting contraction patterns, healthcare providers enhance the quality of care and support optimal labor management. Well-documented patterns provide a valuable resource for assessing labor progress, evaluating interventions, and making informed decisions to promote the safety and well-being of both the mother and the baby.