Benefits of EHR Technology
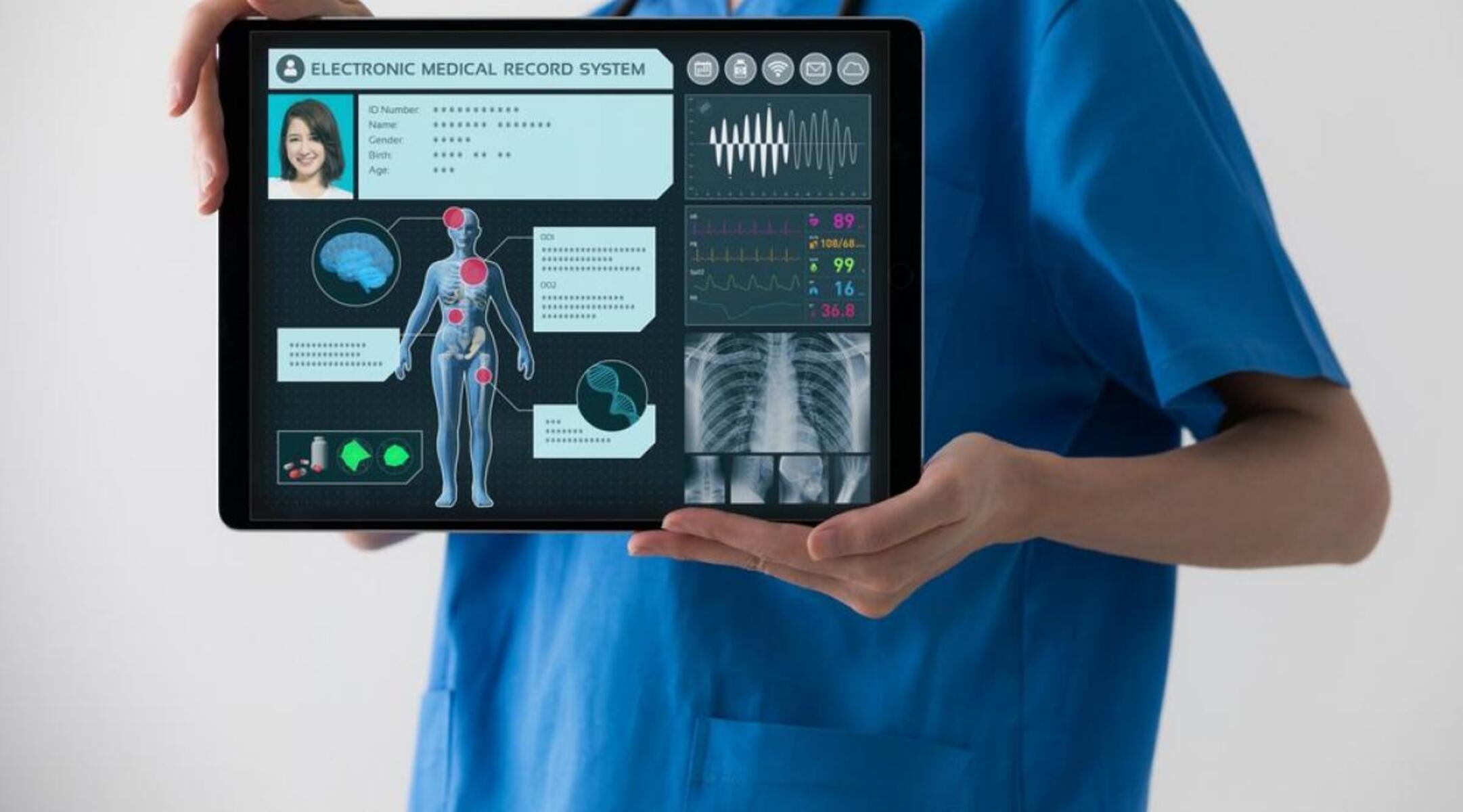
Electronic Health Record (EHR) technology has revolutionized the healthcare industry, offering numerous advantages over traditional paper-based systems. From improved patient care to enhanced efficiency, let’s explore some of the key benefits of utilizing EHR technology:
1. Streamlined Information Access: EHR systems provide healthcare professionals with instant access to an individual’s complete medical history, regardless of their location. This ensures that accurate and comprehensive patient information is readily available, enabling practitioners to make well-informed decisions about diagnosis, treatment plans, and medication management.
2. Increased Efficiency and Productivity: By digitizing medical records, EHR technology eliminates the need for manual paperwork and significantly reduces administrative tasks. Healthcare providers can easily retrieve patient records, schedule appointments, and submit insurance claims, allowing them to spend more time focused on delivering quality care.
3. Improved Patient Care and Safety: EHR systems support better clinical decision-making by providing real-time access to lab results, medication histories, and allergy information. This not only helps in diagnosing and treating patients accurately but also reduces the risk of medication errors, adverse reactions, and duplicate tests.
4. Enhanced Communication and Collaboration: EHR technology facilitates seamless communication and collaboration among healthcare providers, specialists, and patients. It allows for secure sharing of medical information, electronic referrals, and consultation requests, promoting coordinated care and ensuring everyone is on the same page regarding a patient’s healthcare needs.
5. Cost Savings: Adopting EHR technology can result in significant cost savings for healthcare organizations. It eliminates the need for printing and storing paper records, reduces transcription costs, and minimizes the risk of lost or misplaced files. Additionally, streamlined workflows and faster access to information can lead to improved operational efficiency and financial management.
6. Data Analytics and Research: EHR systems offer invaluable data analytics capabilities, allowing healthcare organizations to extract insights and trends from large volumes of patient data. This information can be used to identify population health trends, personalize treatment programs, and make evidence-based decisions for better patient outcomes.
7. Patient Empowerment: EHR technology empowers patients by giving them access to their own health records, test results, and appointment schedules. This promotes patient engagement, enables self-management, and facilitates informed decision-making in collaboration with healthcare professionals.
With these benefits in mind, it’s clear that EHR technology has the potential to transform healthcare delivery, improve patient outcomes, and streamline administrative processes. Its continued adoption and implementation will play a vital role in shaping the future of healthcare.
Components of EHR Systems
An Electronic Health Record (EHR) system consists of various essential components that work together to create a comprehensive and interconnected healthcare information system. Let’s delve into the key components of EHR systems:
1. Patient Demographics: This component includes all the basic information about a patient, such as name, age, gender, contact details, and medical identification numbers. Accurate patient demographics are crucial for identifying and managing individual health records effectively.
2. Medical History: The medical history component captures a patient’s complete health record, including past illnesses, surgeries, allergies, medications, immunizations, and family medical history. It provides healthcare professionals with crucial insights into a patient’s health background and aids in making informed treatment decisions.
3. Clinical Notes: Clinical notes encompass healthcare providers’ observations, diagnoses, treatment plans, and progress reports. These notes are important for ongoing patient care and serve as a communication tool between healthcare professionals involved in the patient’s treatment.
4. Laboratory and Radiology Results: EHR systems allow for the integration of laboratory and radiology results, enabling the storage, retrieval, and presentation of these diagnostic test reports. Having access to these results within the EHR system eliminates the need for physical documents and ensures easy reference during patient consultations.
5. Medication Management: This component tracks a patient’s current and previous medications, including prescriptions, dosage instructions, and medication history. It helps prevent medication errors, identifies potential drug interactions, and supports medication reconciliation during transitions of care.
6. Allergy and Immunization Records: EHR systems maintain comprehensive records of a patient’s known allergies and immunization history. This information is crucial for avoiding allergic reactions and ensuring that patients are up-to-date with recommended vaccinations.
7. Clinical Decision Support (CDS): CDS tools provide healthcare professionals with real-time clinical guidance and evidence-based recommendations within the EHR system. These alerts and reminders help improve patient safety, enhance diagnostic accuracy, and support adherence to best practices and guidelines.
8. Electronic Prescribing: EHR systems enable electronic prescribing, allowing healthcare providers to electronically send prescriptions directly to pharmacies. This component enhances medication safety, reduces errors, and streamlines the prescription refill process.
9. Data Security and Privacy: EHR systems prioritize data security, employing various measures to safeguard patient health information. This includes user authentication, access control, encryption, and compliance with privacy regulations like HIPAA.
10. Interoperability: Interoperability ensures the seamless exchange and sharing of patient information between different healthcare organizations and EHR systems. It enables care coordination, facilitates transitions of care, and promotes continuity in healthcare delivery.
By incorporating these components, EHR systems provide a comprehensive and holistic view of a patient’s health, enabling healthcare professionals to deliver efficient and personalized care. The integration and effective utilization of these components contribute to the successful adoption and implementation of EHR technology.
How EHR Technology Works
Electronic Health Record (EHR) technology operates on a complex and interconnected system that enables the electronic management and sharing of patient health information. Let’s explore the key processes involved in how EHR technology works:
Data Capture: EHR systems are designed to capture patient health information from various sources. This includes manual data entry by healthcare professionals, integration with medical devices for direct data input, importing of external medical records, and receiving electronic data from labs, pharmacies, and other healthcare providers.
Data Storage: Once captured, the patient health information is securely stored in electronic databases within the EHR system. The information is typically organized in a structured and standardized format, allowing for easy searching and retrieval.
Data Accessibility: EHR systems enable authorized healthcare providers to access patient information from any location with an internet connection. This ensures seamless access to medical records, allowing for quick decision-making and coordinated care across different healthcare settings.
Data Integration: EHR technology integrates various components of patient health information, consolidating medical records into a single electronic file. This eliminates the need for paper files and facilitates a comprehensive view of a patient’s health history.
Data Interoperability: Interoperability ensures the smooth exchange of patient health information between different healthcare systems and organizations. EHR technology utilizes health information exchange standards, such as HL7 and FHIR, to facilitate the secure and interoperable sharing of data.
Data Security: EHR systems employ robust security measures to safeguard patient health information. This includes user authentication, access controls, encryption, audit logs, and compliance with privacy regulations. Data security protocols are vital to maintain the confidentiality and integrity of patient records.
Data Analysis and Reporting: EHR technology offers advanced data analysis capabilities, allowing healthcare organizations to extract valuable insights and trends from vast amounts of patient data. This information can be utilized for research, quality improvement initiatives, population health management, and reporting to regulatory bodies.
Data Backup and Recovery: EHR systems implement regular data backup processes to prevent data loss. This ensures that critical patient information is protected from system failures, natural disasters, or other unforeseen events. In the event of data loss, timely recovery processes are in place to restore the information.
Data Privacy and Consent: EHR technology adheres to strict privacy regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), to ensure the privacy and confidentiality of patient information. Patients have control over their data and must provide consent for its sharing and use.
Data Management and Maintenance: EHR systems require ongoing management and maintenance to ensure optimal performance. This includes software updates, database maintenance, system configurations, and periodic data audits to ensure accuracy and completeness.
By understanding how EHR technology works, healthcare professionals can effectively utilize these systems to improve patient care, streamline processes, and enhance the overall efficiency of healthcare delivery. Continued advancements in EHR technology hold great promise for the future of healthcare and patient outcomes.
Features of EHR Systems
Electronic Health Record (EHR) systems are equipped with a range of features and functionalities that enhance the management and accessibility of patient health information. These features contribute to efficient and effective healthcare delivery. Let’s explore some of the key features of EHR systems:
1. Patient Records Management: EHR systems provide a centralized repository for storing and managing patient health records. This includes demographic details, medical history, test results, medications, allergies, and more. Healthcare providers can easily navigate and update these records as needed.
2. Clinical Decision Support: EHR systems offer clinical decision support tools, such as alerts, reminders, and clinical guidelines. These tools help healthcare professionals make evidence-based decisions, identify potential drug interactions or allergies, and optimize treatment plans.
3. E-Prescribing: EHR systems enable electronic prescribing, eliminating the need for paper prescriptions. Healthcare providers can quickly and accurately send prescriptions to pharmacies, improving medication safety and reducing errors.
4. Interoperability: EHR systems facilitate the exchange of health information between different healthcare systems and providers. This interoperability allows for seamless sharing of patient data, promoting continuity of care and eliminating the need for duplicate tests or manual data transfer.
5. Clinical Documentation: EHR systems offer features for easy and efficient clinical documentation. Healthcare providers can electronically record patient encounters, diagnoses, treatment plans, and progress notes. This streamlines the documentation process and ensures accurate and comprehensive record-keeping.
6. Order Management: EHR systems enable the electronic ordering of various healthcare services, such as lab tests, imaging studies, and referrals. This feature helps track and manage these orders, ensuring timely follow-up and reducing administrative burdens.
7. Workflow Management: EHR systems provide tools to optimize workflow and streamline administrative tasks. This includes appointment scheduling, patient registration, billing, and insurance claim submission. These features enhance operational efficiency and save time for healthcare providers.
8. Data Security and Privacy: EHR systems prioritize the security and privacy of patient health information. They employ robust security measures, such as user authentication, encryption, and access controls. Compliance with privacy regulations ensures that patient data is protected from unauthorized access and breaches.
9. Data Analytics: EHR systems offer advanced data analytics capabilities, allowing healthcare organizations to analyze and derive meaningful insights from patient data. These insights can be used for population health management, quality improvement initiatives, and research.
10. Patient Engagement: EHR systems include features that promote patient engagement and empowerment. This may include patient portals, where individuals can access their health records, schedule appointments, communicate with healthcare providers, and participate in their own care decisions.
EHR systems continue to evolve with new features and functionalities that aim to improve patient care, enhance healthcare outcomes, and streamline administrative processes. The utilization of these features supports healthcare professionals in delivering high-quality, patient-centered care and contributes to the advancement of the healthcare industry.
Advantages of EHR Technology
Electronic Health Record (EHR) technology offers a wide range of advantages that significantly enhance healthcare delivery, patient care, and operational efficiency. Let’s explore some of the key advantages of using EHR technology:
1. Improved Accessibility and Availability: EHR systems provide healthcare professionals with instant access to patient information, regardless of their location. This allows for quick and accurate decision-making, even in emergency situations, ultimately improving patient outcomes.
2. Enhanced Patient Safety: EHR technology helps prevent errors in medication management by providing real-time alerts for drug interactions, allergies, and dosage instructions. This reduces the risk of adverse events, improves patient safety, and enhances the quality of care.
3. Streamlined Workflow and Efficiency: By eliminating paper-based processes and automating administrative tasks, EHR technology streamlines workflow and improves operational efficiency. Healthcare providers can spend more time on patient care, leading to increased productivity and reduced administrative burdens.
4. Comprehensive and Accurate Documentation: EHR systems offer structured templates and tools for documenting patient encounters, diagnoses, and treatment plans. This results in more comprehensive, standardized, and accurate documentation, facilitating improved communication and continuity of care.
5. Secure Sharing of Health Information: EHR technology enables secure exchange and sharing of patient information between healthcare providers, specialists, and facilities. This facilitates care coordination, reduces duplicate tests, and ensures that all providers have access to the most up-to-date and relevant patient data.
6. Cost Savings: Implementation of EHR technology can lead to significant cost savings in the long run. It eliminates the need for paper-based processes, reduces transcription costs, minimizes the risk of lost or misplaced files, and optimizes resource utilization.
7. Data Analytics and Insights: EHR systems provide valuable data analytics capabilities, enabling healthcare organizations to extract insights and trends from large amounts of patient data. This information can be used to identify population health patterns, improve care quality, and support evidence-based decision-making.
8. Patient Engagement and Empowerment: EHR technology promotes patient engagement by providing individuals with access to their own health records, appointment scheduling, and communication with healthcare providers. This enhances the patient experience, encourages self-management, and facilitates collaborative decision-making.
9. Continuity of Care: EHR systems ensure that patient information is readily available during transitions of care, such as hospital transfers or referrals to specialists. This promotes continuity of care, reduces the risk of medical errors, and improves care coordination.
10. Environmental Sustainability: Utilizing EHR technology results in reduced paper usage and contributes to environmental sustainability. By transitioning to digital records, healthcare organizations can make a positive impact on the environment and support eco-friendly practices.
EHR technology continues to evolve and revolutionize healthcare delivery. The advantages it offers in terms of accessibility, safety, efficiency, and patient engagement highlight the significant impact it has on shaping the future of healthcare.
Challenges of EHR Implementation
The implementation of Electronic Health Record (EHR) systems, while beneficial, presents several challenges that healthcare organizations must address. Understanding and addressing these challenges can directly impact the success and smooth transition to EHR technology. Let’s explore some of the key challenges involved in EHR implementation:
1. Cost: Implementing EHR systems can be a significant financial investment. Costs include purchasing the software, hardware, training staff, and ongoing maintenance expenses. Healthcare organizations must carefully plan and budget for these costs to ensure a successful implementation.
2. Training and User Adoption: Transitioning from paper-based records to EHR systems requires comprehensive training for healthcare professionals and staff. Resistance to change and lack of comfort with technology can hinder user adoption. Ensuring proper training and support is essential to overcome these challenges and encourage user acceptance.
3. Workflow Disruptions: EHR implementation can disrupt existing workflows, leading to temporary slowdowns in productivity and patient care. Healthcare organizations must carefully plan the implementation process, align workflows with the new system, and provide adequate support to minimize disruptions.
4. Data Conversion and Migration: Migrating existing paper records and historical data into the EHR system can be a complex and time-consuming process. Ensuring the accuracy and integrity of the data during conversion is crucial. Healthcare organizations must develop comprehensive data migration strategies and closely monitor the process to maintain data quality.
5. Interoperability Challenges: The ability of EHR systems to successfully exchange and share patient data with other healthcare systems is crucial for care coordination. However, achieving interoperability between different EHR systems and healthcare providers remains a challenge. Healthcare organizations need to work collaboratively and implement industry standards to overcome interoperability hurdles.
6. Privacy and Security Concerns: Protecting patient health information is of utmost importance. EHR systems must comply with strict privacy and security regulations like HIPAA to safeguard sensitive data. Healthcare organizations must invest in robust security measures, training, and ongoing monitoring to mitigate privacy and security risks.
7. Continuity and Availability of Service: EHR system downtime can disrupt the delivery of patient care and cause inconvenience to healthcare providers. Ensuring a reliable infrastructure, implementing backup systems, and developing contingency plans are essential to minimize the impact of system outages and ensure continuous access to patient information.
8. Vendor Selection: Choosing the right EHR vendor that aligns with the organization’s needs and goals can be a challenge. Adequate research, vendor demonstrations, and due diligence are necessary to make an informed decision and ensure long-term compatibility and support.
9. Change Management: Implementing EHR systems involves organizational change. Successfully managing this change requires effective leadership, communication, and stakeholder engagement. Healthcare organizations must actively involve staff in the planning and decision-making process to gain buy-in and support for the implementation.
10. Regulatory and Legal Considerations: EHR implementation must adhere to various regulatory requirements, such as data privacy and consent. Healthcare organizations must stay updated on evolving regulations and legal considerations to avoid compliance issues and potential penalties.
By proactively addressing these challenges, healthcare organizations can navigate the EHR implementation process more effectively, maximizing the benefits and ensuring a successful transition to digital healthcare records.
EHR Interoperability
EHR interoperability refers to the ability of different Electronic Health Record (EHR) systems to seamlessly exchange and share patient health data across various healthcare organizations and providers. Achieving interoperability is crucial for effective care coordination, continuity of care, and improved patient outcomes. Let’s explore the key aspects and benefits of EHR interoperability:
1. Data Exchange: Interoperability enables the secure exchange of patient health information between different EHR systems. This allows healthcare providers to access comprehensive and up-to-date patient records, regardless of where the initial records were created. Health information exchange ensures that healthcare professionals have the necessary data to make informed decisions and provide quality care.
2. Care Coordination: EHR interoperability facilitates seamless care coordination among healthcare providers. When different providers can access the same patient records, transitions of care become smoother. This reduces the risk of medical errors, duplicate tests, and unnecessary treatments, leading to better patient outcomes and enhanced patient satisfaction.
3. Continuity of Care: Interoperability ensures that patient information is available wherever and whenever it is needed. When patients move between healthcare settings or receive care from different providers, interoperable EHR systems ensure that important medical history, diagnoses, medications, and treatment plans can be accessed and shared. This promotes continuity of care and helps prevent gaps in healthcare delivery.
4. Efficiency and Cost Savings: EHR interoperability streamlines workflows and reduces administrative burdens. Healthcare professionals can readily access and share patient data, leading to more efficient care coordination, improved communication, and reduced reliance on manual data entry and paper-based records. This enhances operational efficiency and can result in cost savings for healthcare organizations.
5. Enhanced Decision-Making: Interoperability allows healthcare professionals to access a patient’s complete health record, including information from different providers and healthcare facilities. Having a comprehensive view of a patient’s medical history, allergies, medications, and test results enables better clinical decision-making. This leads to more accurate diagnoses, personalized treatment plans, and improved patient outcomes.
6. Patient Empowerment: Interoperability in EHR systems empowers patients by giving them control over their health information. Patients can access their records, securely communicate with healthcare providers, and actively participate in their own care decisions. This increased engagement and access to information promotes patient satisfaction and facilitates better health outcomes.
7. Research and Population Health Management: Interoperability enables the aggregation of large sets of de-identified patient data for research and population health management purposes. When EHR systems can exchange data seamlessly, it becomes easier for healthcare organizations to analyze health trends, identify disease patterns, and improve public health interventions.
Despite the numerous benefits, achieving full EHR interoperability remains a challenge. Different EHR systems often use different data formats, coding systems, and information exchange standards. Healthcare organizations, EHR vendors, and regulatory bodies must work collaboratively to establish and implement interoperability standards, such as HL7 and FHIR. Efforts to address privacy and security concerns and overcome technical and structural barriers are essential for achieving widespread interoperability in the future of healthcare.
Privacy and Security Considerations
As Electronic Health Record (EHR) technology becomes more prevalent in healthcare settings, ensuring the privacy and security of patient health information is of paramount importance. Healthcare organizations must address various privacy and security considerations to protect sensitive data from unauthorized access, breaches, and misuse. Let’s explore some key aspects of privacy and security in EHR systems:
1. Data Encryption: EHR systems employ encryption techniques to safeguard patient data. Encryption converts data into an unreadable format during transmission or storage, making it less susceptible to unauthorized access. Strong encryption protocols ensure the confidentiality and integrity of patient information.
2. Access Control: EHR systems implement access controls to limit data access based on users’ roles, responsibilities, and authentication credentials. Role-based access control ensures that only authorized individuals can view, modify, or delete specific patient records, reducing the risk of unauthorized data access or data breaches.
3. User Authentication: EHR systems require strong user authentication mechanisms, such as passwords, two-factor authentication, or biometric authentication, to verify the identity of users. This helps ensure that only authorized individuals can access patient information, reducing the risk of data breaches caused by compromised credentials.
4. Audit Trail: EHR systems maintain an audit trail, which records all activities and transactions related to patient records. This includes user access, modifications, and data exchanges. Audit trails help detect and investigate any unauthorized or suspicious activities, allowing for prompt action in case of security incidents.
5. Training and Awareness: Healthcare organizations must provide comprehensive training and ongoing awareness programs to all employees regarding privacy and security protocols. This helps ensure that staff members understand their responsibilities in safeguarding patient data and are aware of potential security threats, phishing attempts, and best practices for data protection.
6. Regulatory Compliance: EHR systems must comply with privacy and security regulations, such as the Health Insurance Portability and Accountability Act (HIPAA). Healthcare organizations must establish policies and procedures that align with these regulations to protect patient privacy, facilitate secure data exchange, and mitigate the risk of non-compliance penalties.
7. Data Breach Response: In the event of a data breach or security incident, healthcare organizations must have incident response plans in place. This includes procedures for identifying, containing, and mitigating the impact of the breach. Prompt notification of affected individuals, regulatory authorities, and timely remediation actions are essential to minimize the consequences of a breach.
8. Physical and Environmental Safeguards: EHR systems require physical and environmental safeguards to protect the infrastructure housing patient information. This includes secure data centers, power backup systems, fire suppression measures, and secure network connections. These safeguards help prevent physical theft, damage, or unauthorized access to data.
9. Business Associate Agreements: EHR systems often involve business associates, such as cloud service providers or third-party vendors. Healthcare organizations should establish legally binding agreements to ensure that these associates adhere to privacy and security standards, maintain data confidentiality, and report any breaches or security incidents promptly.
10. Ongoing Security Audits and Assessments: Healthcare organizations should conduct regular security audits and risk assessments to identify vulnerabilities and areas for improvement. This ensures that security controls are up to date, addresses emerging threats or regulatory changes, and maintains a proactive approach to information security.
By prioritizing privacy and security considerations, healthcare organizations can build a robust framework for protecting patient data in EHR systems. Addressing these considerations helps foster trust among patients, ensures legal compliance, and supports the confidentiality and integrity of electronic health records.
EHR Technology in Healthcare Settings
Electronic Health Record (EHR) technology has become an integral part of healthcare settings, transforming the way patient information is managed and shared. EHR systems are now widely adopted across a range of healthcare settings, including hospitals, clinics, private practices, and long-term care facilities. Let’s explore how EHR technology is utilized in these settings:
1. Hospitals: EHR systems are extensively used in hospitals, where they facilitate seamless access to patient information across various departments and specialties. This enables healthcare providers to deliver coordinated and patient-centric care. EHRs in hospitals streamline workflows, support clinical decision-making, and ensure efficient communication among healthcare teams.
2. Clinics and Private Practices: EHR systems are increasingly common in clinics and private practices. They allow healthcare providers to efficiently manage patient records, streamline administrative tasks, and enhance the overall patient experience. EHRs in these settings enable providers to easily schedule appointments, view patient histories, order tests, and electronically prescribe medications, improving efficiency and accuracy in care delivery.
3. Ambulatory Care Centers: Ambulatory care centers, such as urgent care facilities, use EHR systems to manage patient information and provide timely care. EHRs in these settings facilitate quick access to patient records, support decision-making, and enhance patient flow management. The interoperability of EHRs enables seamless sharing of patient information with other healthcare providers, ensuring continuity of care.
4. Long-Term Care Facilities: EHR systems are valuable in long-term care facilities, where they help manage complex patient populations. EHRs in these settings support care coordination among various healthcare professionals, aid in medication management, and ensure accurate documentation for patient care plans. The comprehensive patient records stored in EHRs assist in managing chronic conditions and providing personalized care.
5. Specialized Healthcare Facilities: EHR technology is utilized in specialized healthcare facilities, such as mental health clinics, rehabilitation centers, and specialty hospitals. EHRs in these settings cater to the unique needs of the specialties, allowing for specialized assessment tools, treatment plans, and documentation requirements. EHRs facilitate collaborative care across multidisciplinary teams and enhance communication between different specialists.
6. Public Health and Research Institutions: EHR technology is also employed in public health agencies and research institutions. EHRs in these settings provide a wealth of data for population health management, disease surveillance, and research. EHRs support public health initiatives, enabling better monitoring of disease outbreaks, epidemiological investigations, and evidence-based research.
EHR technology continues to advance and play an essential role in healthcare settings. It improves accessibility to patient information, enhances communication, and supports coordinated care. Implementing and optimizing EHR systems in diverse healthcare settings contributes to better patient outcomes, increased operational efficiency, and improved overall healthcare delivery.
Future of EHR Technology
The future of Electronic Health Record (EHR) technology holds tremendous potential to revolutionize healthcare delivery and enhance patient care. As technology continues to advance, several key trends and developments are shaping the future of EHR systems. Let’s explore what lies ahead for EHR technology:
1. Interoperability and Data Exchange: Achieving seamless interoperability between different EHR systems remains a top priority. The industry is moving towards standardizing data exchange formats and protocols, such as Fast Healthcare Interoperability Resources (FHIR). This will allow for secure and efficient sharing of patient health information across healthcare organizations and providers, leading to improved care coordination and continuity of care.
2. Artificial Intelligence (AI) Integration: AI technologies, such as machine learning and natural language processing, are increasingly being integrated into EHR systems. AI can assist healthcare professionals in detecting patterns, predicting outcomes, and providing clinical decision support. AI integration in EHRs has the potential to enhance diagnostic accuracy, improve treatment recommendations, and automate administrative tasks to improve workflow efficiency.
3. Patient-centered Design: Future EHR systems will place a greater emphasis on patient-centered design. User experience and patient engagement will be prioritized, with intuitive interfaces, mobile accessibility, and patient portals to empower individuals in managing their own health. Patient-generated data, such as wearables and personal health apps, may also be integrated into EHRs to provide a comprehensive view of the patient’s health.
4. Data Analytics and Population Health Management: EHR systems will continue to advance in their data analytics capabilities. With the increasing amount of patient data available, healthcare organizations can leverage EHRs to identify population health trends, personalize treatment plans, and measure outcomes. EHRs will play a significant role in supporting population health management initiatives and preventive care.
5. Telehealth Integration: The COVID-19 pandemic has accelerated the adoption of telehealth services. In the future, EHR systems will integrate seamlessly with telehealth platforms, allowing for virtual consultations, remote patient monitoring, and secure video conferencing. Telehealth integration in EHRs will enhance access to care, improve patient convenience, and support remote healthcare delivery.
6. Enhanced Data Security: As cyber threats continue to evolve, future EHR systems will implement even stronger security measures to protect patient health information. This includes advanced encryption techniques, robust access controls, and real-time monitoring for potential security breaches. Blockchain technology may also find application in securing EHRs, ensuring data integrity and privacy.
7. Personalized Medicine: EHR systems will play a crucial role in advancing personalized medicine approaches. By integrating genomic data, pharmacogenomic information, and patient-specific factors, EHRs will support individualized treatment plans and targeted therapies. This will result in more effective and tailored healthcare interventions.
8. Voice Recognition and Natural Language Processing: EHR systems will increasingly incorporate voice recognition and natural language processing capabilities. This will allow healthcare providers to dictate clinical notes and documentation, reducing administrative burden and enhancing efficiency. Natural language processing will also assist in extracting meaningful insights from unstructured medical data.
The future of EHR technology is focused on improving healthcare outcomes, enhancing patient experiences, and streamlining healthcare workflows. By embracing these advancements and addressing challenges proactively, EHR systems will continue to evolve, transforming healthcare delivery and shaping the future of medicine.